Already in its fourth year, the humanitarian response in the world’s largest refugee camp is gearing towards a protracted crisis. With the funding support from the Government of Bangladesh/World Bank, WHO and health partners are transforming donations into action to address existing gaps in health services in Cox’s Bazar in an effort to sustain the achievements made since 2017 and to further support the government led health response in the district.
The Additional Financing for the Health Sector Support Project received $5.5 Million from the Government of Bangladesh/World Bank for three years (2019-22) to accelerate the work on capacity building and ensuring provision of essential services in 45 designated health care facilities in Cox’s Bazar through a strategic multi-sectoral approach.
The underlying principle of this three-year plan is to support national health institutions in delivering an effective response and increase direct investment in local public health institutions.
 Joint Secretary (Planning), Medical Education and Family Welfare Division, Ministry of Health and Family Welfare (MoHFW); Mr Mohammad Abdus Salam Khan; WHO Deputy Representative, Dr Bhupinder Kaur Aulakh; Upazila Health and Family Planning Officer at Teknaf Upazila Health Complex (UHC), Dr. Tito Chandra Shil; MoHFW Coordination Cell Chief Coordinator, Professor Brig. Gen Rtd. Mohammad Ali; and other dignitaries, commissioning the Conference Hall at Teknaf UHC - WHO Bangladesh
Joint Secretary (Planning), Medical Education and Family Welfare Division, Ministry of Health and Family Welfare (MoHFW); Mr Mohammad Abdus Salam Khan; WHO Deputy Representative, Dr Bhupinder Kaur Aulakh; Upazila Health and Family Planning Officer at Teknaf Upazila Health Complex (UHC), Dr. Tito Chandra Shil; MoHFW Coordination Cell Chief Coordinator, Professor Brig. Gen Rtd. Mohammad Ali; and other dignitaries, commissioning the Conference Hall at Teknaf UHC - WHO Bangladesh
Transforming funding into action, WHO has been supporting the government led health response at the various fronts of the Rohingya refugee humanitarian response. The project is funded by the Government of Bangladesh/World Bank having been launched in 2018 to support 45 health care facilities in the refugee camps and nearby host community deliver quality health services in collaboration with four UN agencies: IOM, UNICEF, UNFPA and WHO.
The World Health Organization (WHO) started implementing this project in March 2019 with the recruitment of 22 technical and support personnel which were deployed to the Ministry of Health and Family Welfare (MoHFW), Directorate General of Health Services (DGHS), Directorate General of Family Planning (DGFP) in Dhaka and to the MoHFW Coordination Cell in Cox’s Bazar. Together, the support staff have been contributing to enhance coordination and monitoring capacity in the humanitarian response.
 Joint Secretary (Planning), Medical Education and Family Welfare Division (ME&FWD), MoHFW Mr Mohammad Abdus Salam Khan; WHO Deputy Representative, Dr Bhupinder Kaur Aulakh; and WHO Public Health Response Consultant, Dr Simon Kaddu Ssentamu examining a Noncommunicable Diseases (NCDs) register (developed by WHO) that is being piloted at Baharchora Family Welfare Center (FWC) for risk-based assessment in the management of patients with NCDs - WHO Bangladesh
Joint Secretary (Planning), Medical Education and Family Welfare Division (ME&FWD), MoHFW Mr Mohammad Abdus Salam Khan; WHO Deputy Representative, Dr Bhupinder Kaur Aulakh; and WHO Public Health Response Consultant, Dr Simon Kaddu Ssentamu examining a Noncommunicable Diseases (NCDs) register (developed by WHO) that is being piloted at Baharchora Family Welfare Center (FWC) for risk-based assessment in the management of patients with NCDs - WHO Bangladesh
As part of the Additional Financing for the Health Sector Support Project, WHO is providing capacity building to enhance the government’s capacity to access updated disease burden information in Cox’s Bazar through its Early Warning, Alert and Response System (EWARS). The system was deployed to Cox’s Bazar only a few days into the refugee crisis in 2017.
The project has been key to respond to the COVID-19 outbreak, comprising support staff, supplies and technical expertise that enabled the Institute of Epidemiology Disease Control and Research (IEDCR) Field Laboratory to ensure large scale testing for COVID-19 in Cox’s Bazar and neighbouring districts with results within 24/48 hours. Testing was coupled by a robust surveillance system which to date has responded to more than 420 COVID-19 alerts through Rapid Investigation and Response Teams (RIRTs).
At healthcare facility level, infection prevention and control, case management and Package of Essential Noncommunicable disease interventions for primary health care providers (PEN) trainings were conducted for partners and government facilities including the provision of Noncommunicable disease (NCD) kits to all 45 health facilities under this project.
WHO is also supporting the implementation of the healthcare waste management plan for the Ukhiya and Teknaf Upazila Health Complexes, 14 Health and Family Welfare posts, 10 Primary Health and Family Welfare care centres, 10 community clinics and nine union facilities, following an assessment conducted in 2019.
 Health care without harm: with the funding support from the Government of Bangladesh/World Bank, WHO developed a comprehensive healthcare waste management plan that created a more environmentally friendly waste management during the COVID-19 response in Ukhiya and Teknaf - WHO Bangladesh
Health care without harm: with the funding support from the Government of Bangladesh/World Bank, WHO developed a comprehensive healthcare waste management plan that created a more environmentally friendly waste management during the COVID-19 response in Ukhiya and Teknaf - WHO Bangladesh
Every three months, the Government of Bangladesh (GoB), WHO and health partners come together to review the progress in implementing the Government of Bangladesh/World Bank funded project which focuses on strengthening the Health Sector while mitigating the impact on the camp and host communities and increasing resilience among these vulnerable communities.
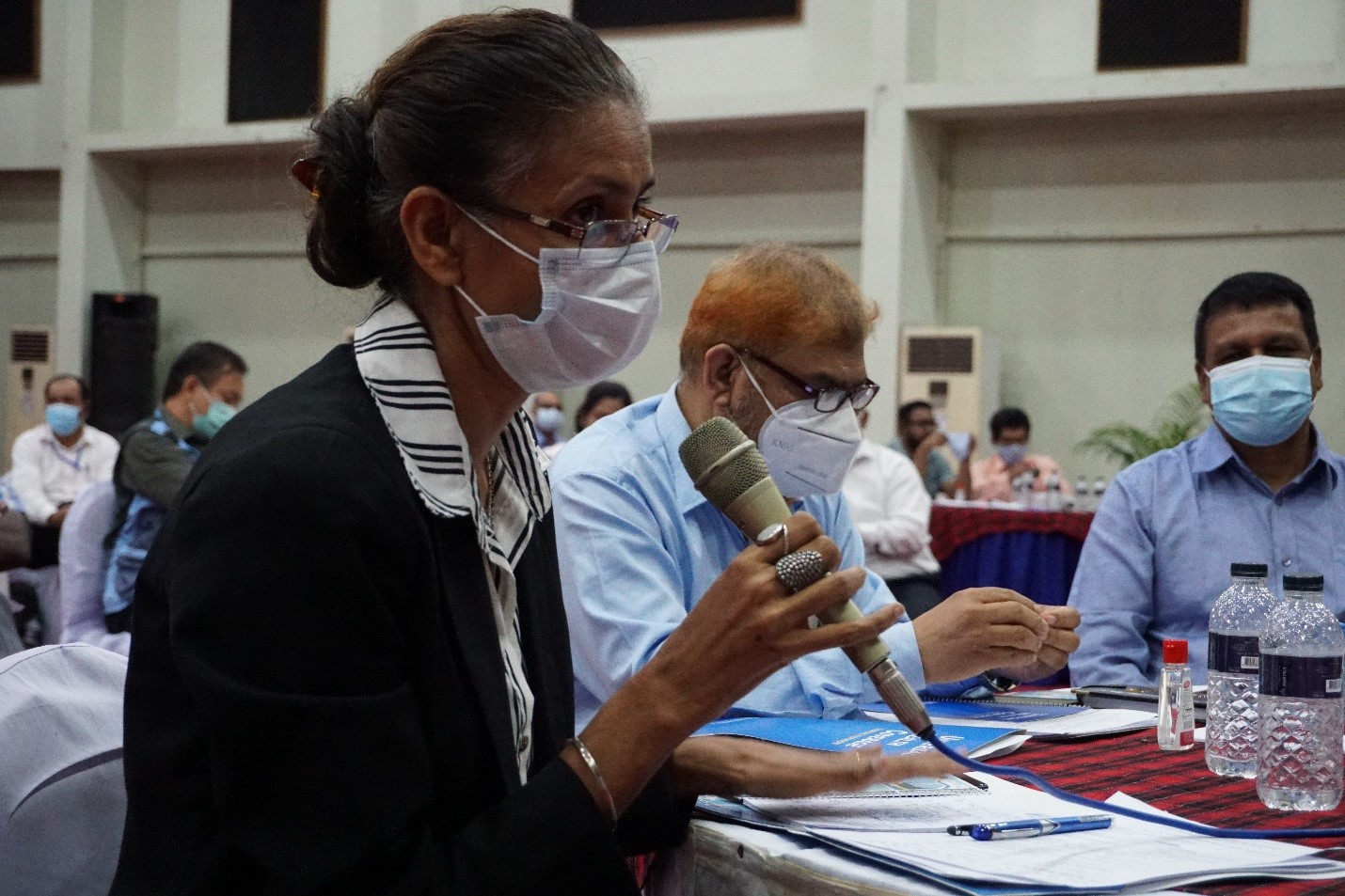 WHO Deputy Representative, Dr Bhupinder Kaur Aulakh, at the workshop held in Cox’s Bazar in September 2020 to review the progress in implementing the Government of Bangladesh/World Bank funded project - WHO Bangladesh
WHO Deputy Representative, Dr Bhupinder Kaur Aulakh, at the workshop held in Cox’s Bazar in September 2020 to review the progress in implementing the Government of Bangladesh/World Bank funded project - WHO Bangladesh
Under the leadership of the Additional Director General (Planning and Development) DGHS, Professor Dr. Meerjady Sabrina Flora, two quarterly coordination and review workshops of this project have been held in Cox’s Bazar. The first, conducted in September 2020, looked into the progress met while addressing challenges that had been compounded since the onset of the COVID-19 pandemic. In February 2021 partners came together to conduct field visits in addition to reviewing progress.
 Director General of Directorate General of Health Service (DGHS), Professor Dr Abul Bashar Mohammad Khurshid Alam, and Additional Director General (Planning and Development) DGHS, Professor Dr Meerjady Sabrina Flora discussing feedback to UN agencies on progress of implementation of the HSSP project - WHO Bangladesh
Director General of Directorate General of Health Service (DGHS), Professor Dr Abul Bashar Mohammad Khurshid Alam, and Additional Director General (Planning and Development) DGHS, Professor Dr Meerjady Sabrina Flora discussing feedback to UN agencies on progress of implementation of the HSSP project - WHO Bangladesh
Using the building blocks of a health care system, WHO and other UN agencies have worked collaboratively to initiate the much-needed development of the health system in Cox’s Bazar. The Health and Gender Support Project (HGSP) will see much more investment in technical capacities of human resources to utilize digital health information systems, especially for NCDs, whilst ensuring real time access to data and timely follow up for patients with chronic conditions.
“Strengthening community outreach activities especially counselling and health education sessions is vital to improve NCD interventions’ outcomes. The same way, building on human resources capacities at all levels will make health systems stronger. I am confident that with the support provided by the MoHFW Coordination Cell, health partners will be able to effectively map the availability of qualified human resources and health services coverage to avoid duplication of efforts”, notes Director General of Health Services, Professor Dr Abul Bashar Mohammad Khurshid Alam.
 Joint Secretary (Planning), ME&FWD, MOHFW, Mr Mohammad Abdus Salam Khan; WHO Representative, Dr Bardan Jung Rana; and WHO Head of Sub-Office, Dr Kai von Harbou, discussing findings from the field visits under Government of Bangladesh/World Bank funded projects - WHO Bangladesh
Joint Secretary (Planning), ME&FWD, MOHFW, Mr Mohammad Abdus Salam Khan; WHO Representative, Dr Bardan Jung Rana; and WHO Head of Sub-Office, Dr Kai von Harbou, discussing findings from the field visits under Government of Bangladesh/World Bank funded projects - WHO Bangladesh
“It is impressive how far we have come with this project given the fact that it has started back in 2018 to establish a coordination and health surveillance mechanism to support the office of the Civil Surgeon in the early days of the Rohingya crisis in Cox’s Bazar. WHO remains committed to support the Government of Bangladesh in delivering quality services to the vulnerable communities in the district”, says WHO Representative, Dr Bardan Jung Rana.
Firmly present in the country since 1972, WHO has been supporting Bangladesh to navigate the challenges posed in the provision and maintenance of essential health services and to create opportunities to provide affordable and quality services for the prevention and management of NCDs and mental disorders in primary health care (PHC) facilities, to name a few, as these are key to achieving universal health care (UHC).
