Infection prevention and control (IPC) and water, sanitation and hygiene (WASH) in health emergencies
Infection Prevention and Control (IPC) and Water, Sanitation, and Hygiene (WASH) are critical enablers of safe, scalable, and high-quality health service delivery across all phases of public health and humanitarian emergencies. These pillars ensure the protection of patients, health workers, and communities by preventing health-care-associated infections (HAIs) and reducing the risk of disease transmission in both health care and community settings.
During public health emergencies, the rapid scale-up of health services can strain systems and increase the risk of adverse events. Reinforcing IPC and WASH capacities is essential to maintaining continuity of care, enabling safe clinical scale-up, and mitigating amplification of infectious disease outbreaks. This is particularly crucial in humanitarian settings where basic IPC and WASH systems are often lacking or disrupted.
Beyond health-care facilities, the availability of safe water, sanitation, and hygiene infrastructure is equally vital in community settings, such as schools, internally displaced people and refugee camps, shelters, places of worship, and prisons, to prevent transmission and protect the public.
The IPC and WASH team delivers strategic, technical, and operational support to integrate IPC and WASH into emergency response operations and broader health system strengthening.
Key functions and strategic priorities for WHE IPC and WASH teams
1. Networks and partnerships
WHO leads and coordinates global platforms to align IPC and WASH in the context of health emergency efforts across stakeholders. Key partnerships include:
2. Country operational support
WHO supports the strengthening of national readiness and response efforts for IPC and WASH, while ensuring continuity of safe, quality care at all levels of the health system through:
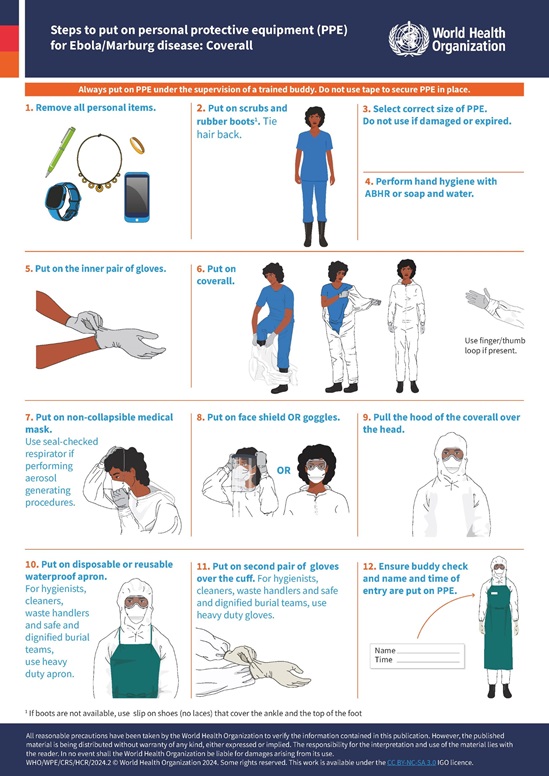
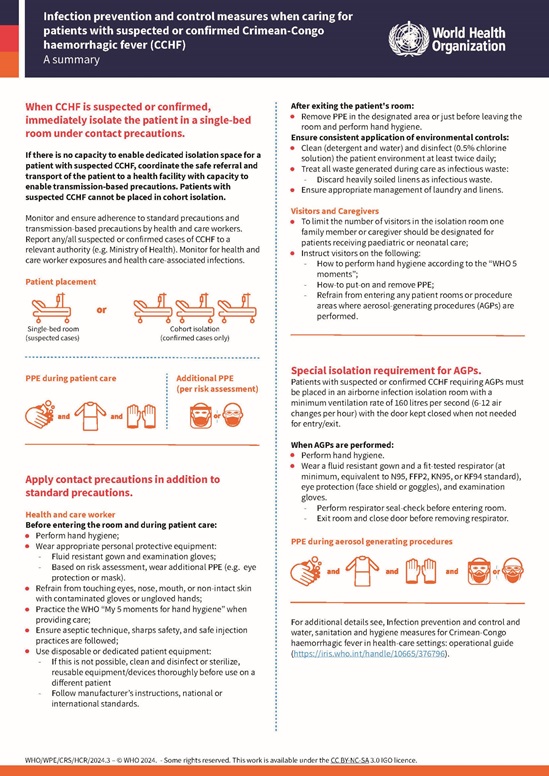
3. Evidence-based technical products
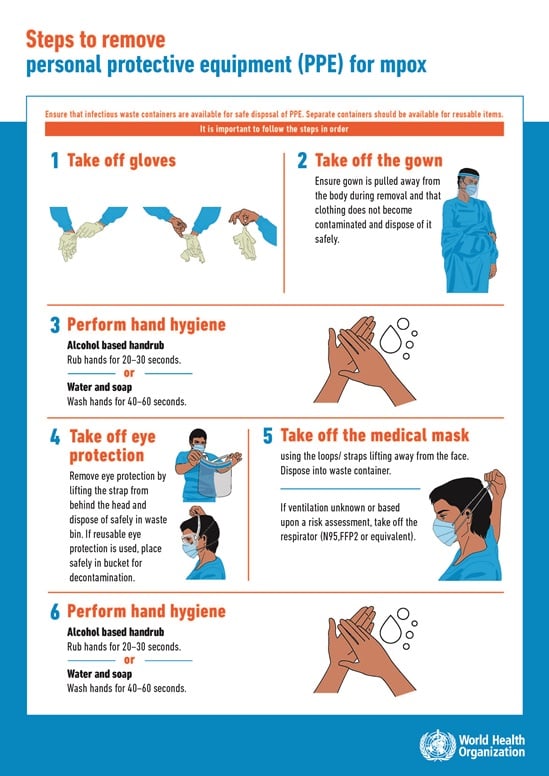
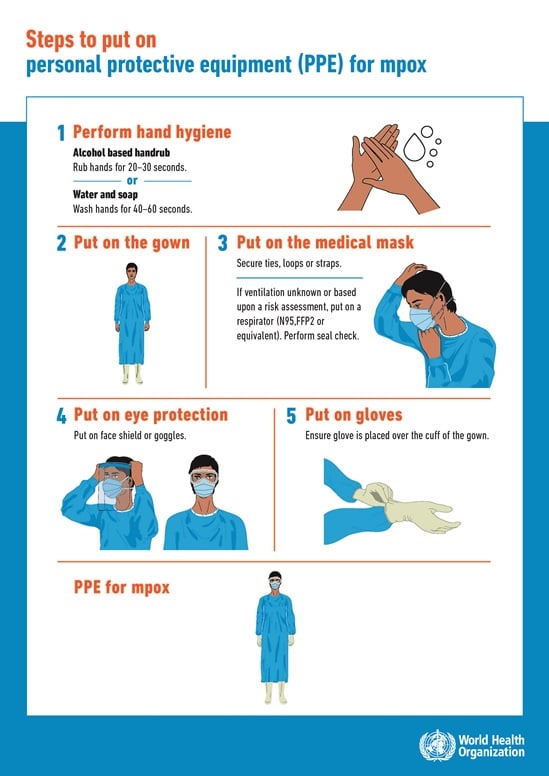
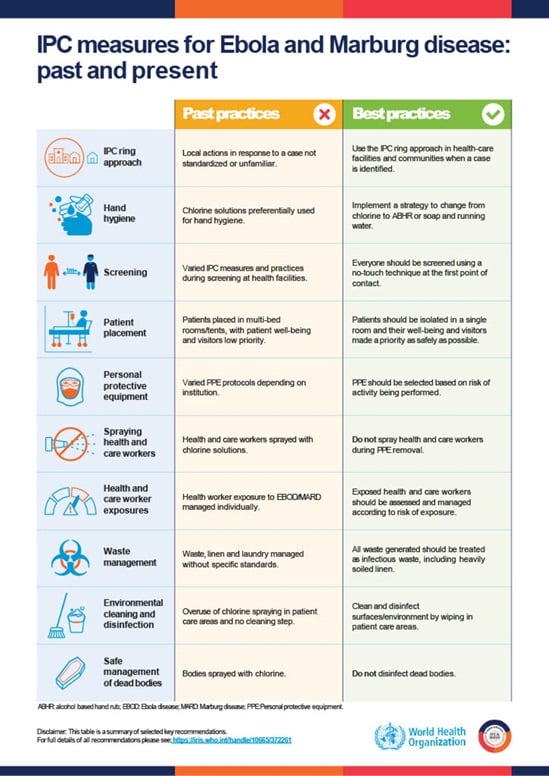
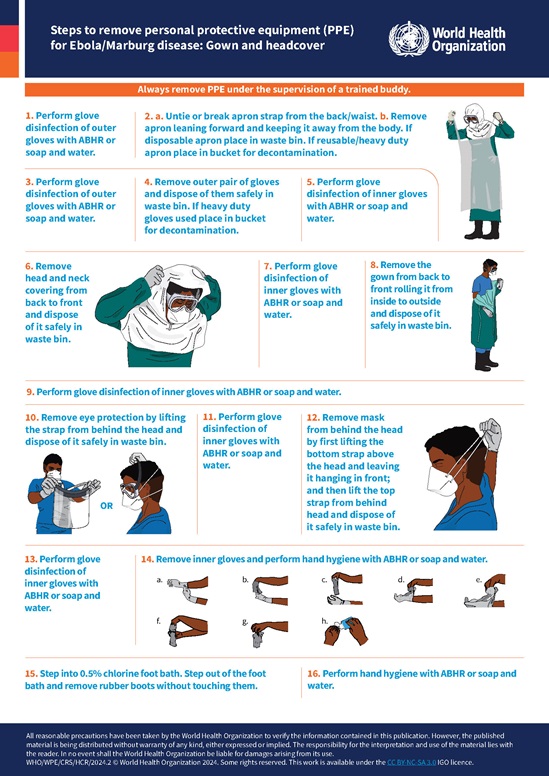
WHO develops and disseminates normative and derivative products to guide effective IPC and WASH implementation in emergency settings through:
4. Capacity building
WHO enables local actors to lead IPC and WASH implementation and ensure sustainability beyond emergency periods through:
5. Research, data, and innovation
WHO promotes decision-making and quality of care through: