
The WHO multisectoral accountability framework for TB (MAF-TB): progress in adaptation and implementation
Tuberculosis (TB) remains one of the top infectious killers in the world, and further innovations and multisectoral actions are needed to reach the World Health Organization (WHO) End TB Strategy targets. Despite universal acknowledgement that TB is driven by social and economic determinants, the TB response is still mainly focused on the health sector (1). Multisectoral engagement is critical, given the impact of COVID-19 on health systems and economies worldwide, especially on the poorest people.
The political declaration of the 2018 United Nations (UN) General Assembly high-level meeting on TB (2) includes a commitment by Member States to enable and pursue multisectoral engagement and accountability at global, regional, national and local levels to end TB. The declaration also includes a request to the Director-General of WHO to ensure timely implementation of a multisectoral accountability framework for TB. The WHO Global TB Programme (GTB) subsequently released the Multisectoral accountability framework to accelerate progress to end tuberculosis by 2030 (MAF-TB) in May 2019 (3). The aim of MAF-TB is to support effective collaboration and accountability of governments and stakeholders at all levels to ramp up the response towards ending TB. The framework will help to facilitate multisectoral action, mutual accountability and measurement of progress towards commitments on TB at global, regional, national and subnational levels.
The UN Secretary-General’s 2020 report on progress towards achieving global TB targets and implementation of the UN political declaration on TB (4) also highlights the importance of multisectoral engagement for progress towards ending TB. The report includes a request for WHO to continue supporting Member States to adapt and use the MAF-TB in collaboration with partners, civil society and affected communities, and lead periodic global reviews of the TB response.
Status of MAF-TB adaptation and implementation
WHO provides coordination, guidance and technical support to countries and stakeholders for adapting and implementing MAF-TB, and for monitoring and review at global, regional and country levels.
All three levels of WHO are working closely with various organizations to build capacity, increase awareness and share best practices and experiences of multisectoral engagement and accountability. The collaborating organizations include UN agencies – for example, the International Labour Organization (ILO), International Organization for Migration, UN High Commissioner for Refugees, World Food Programme (WFP) and UN Children’s Fund (UNICEF) – and other partners such as the WHO Civil Society Task Force (CSTF) and civil society and community organizations.
A special WHO portal on MAF-TB, with key resources and opportunities for questions and answers, has been promoted on WHO’s interactive End TB Forum platform, which features several hundred members. The portal helps to share knowledge, relevant information and best practices on MAF-TB implementation and use, and helps to engage different stakeholders and sectors. It is used also for the organization of WHO End TB webinars with a spotlight on MAF-TB, which also engage other UN agencies. Furthermore, WHO co-hosted a conference and is working closely with the Health and Social Protection Action Research and Knowledge Sharing (SPARKS) network to improve social protection approaches in the context of the COVID-19 pandemic (5).
Based on the WHO global data collected in 2021 (Table 1) there has been notable progress in MAF implementation. A total 157 countries, including almost all (29) high TB burden countries, published annual TB reports on progress toward national TB-related targets and commitments. National mechanisms for high-level review of progress towards ending TB have been established in 125 countries, 19 of which are high TB burden countries. Civil society and affected communities are actively engaged in the multisectoral accountability and review processes in 87 countries, 15 of which are high TB burden countries.
WHO regional offices are working closely with WHO country offices, civil society representatives and partners to provide technical support to the countries in implementation of MAF-TB. In 2020–2021, with the support from the WHO Regional Office for Europe, five pilot countries (Belarus, Moldova, Kazakhstan, Tajikistan and Ukraine) initiated operationalization and adaptation of the MAF-TB to their national context. Box 1 presents four country case studies and Box 2 highlights examples of national multisectoral actions for the social protection of people with TB supported by UN agencies.
Findings from the MAF-TB baseline assessment, 2021
To facilitate the implementation of MAF-TB at country level, WHO developed the MAF-TB checklist (6) and supported baseline assessments. Results from the assessments inform further steps to adapt and implement MAF-TB at national level.
Global TB Programme analysis and evaluation of the MAF-TB baseline assessment in 45 responding countries indicates progress in implementation of the four essential MAF-TB components (commitments, actions, monitoring and reporting, and review). All four components are in place in 17 of the 45 countries included in the MAF-TB baseline assessment (Fig. 1).
Thirty countries reported on the translation into national policies of targets from the Sustainable Development Goals (SDGs), the WHO End TB Strategy or the UN high-level meeting political declaration on TB. Ongoing were normalization of key commitments on strengthening multisectoral accountability mechanisms; pursuing science, research and innovation; and fund mobilization for universal access to TB diagnosis, treatment and care. Ten countries showed examples of concrete actions in place.
Fifteen countries have formalized their national multisectoral coordination mechanisms, while 25 countries have updated their national strategic plans aligned with MAF-TB principles on integration of TB services within primary health care and addressing HIV as a TB risk factor. However, fewer than half of the responding countries have in place the integration of multisectoral actions to address other risk factors and social determinants of TB (e.g. undernutrition and poverty).
Among the 45 countries that participated in the MAF-TB baseline assessment, 40 have a strong TB surveillance system (routine recording and reporting on TB via national information system) in place and are reporting annually to WHO via the global TB data collection system. The latest national assessments of TB surveillance in 29 of the 30 high TB burden countries confirm and complement the findings from the MAF-TB baseline assessments. In particular, 27 countries have surveillance systems that meet WHO requirements for standardization and consistency in the case definitions used and type of data collected. The periodic transmission of data and quarterly reports upstream from subnational levels to national level requires continued attention because only 10 countries have such a system in place. Similarly, fewer than half of the high TB burden countries have either partially or fully transitioned from paper to digital case-based surveillance systems, and 23 countries did not meet the standards related to diagnosis and reporting of data on TB in children. National vital registration (VR) systems with high coverage and coding of causes of death according to international standards is challenging and requires strengthening.
Research and study data to inform planning are increasingly available. Among the countries in the MAF-TB baseline assessment, 24 have national evidence-based data available from surveys and studies such as prevalence, patient cost and drug resistance surveys, and inventory and other special studies.
A total of 36 of the 45 reported countries do not have high-level leadership engagement for the periodic review of the TB response. In about half of the countries included in the baseline assessment, there is no clearly defined list of accountable stakeholders beyond the health sector. Furthermore, relevant indicators for the performance measurement of accountable stakeholders are not set and no budget is assigned for TB-specific activities. In fewer than half of the countries, the TB response is still covered only by the health sector and is the responsibility of the ministry of health (MoH).
Civil society and affected communities, most notably in high TB burden countries, are engaged in all four components of MAF-TB, especially in setting and implementation of commitments. This is consistent with the WHO global data collected in 2021 (Table 1). Engagement in activities related to monitoring and reporting is limited, however – only nine responding countries had set performance indicators to measure civil society engagement in TB response.
In general, countries are progressing in their adaptation and roll-out of the latest WHO guidelines on TB diagnosis and treatment, released between 2016 and 2020, with more than 80% of countries that participated in the MAF-TB baseline assessment making progress. In particular, WHO guidelines on the treatment of drug-resistant TB (7) are implemented in half of the reported countries. According to the WHO global TB data, 90 countries are using all-oral longer TB treatment regimens and 65 are using shorter treatment regimens for multidrug-resistant or rifampicin-resistant TB (MDR/RR-TB).
WHO will continue to provide technical support for country adaptation and implementation of MAF-TB, and will be publishing operational guidance and best practices on MAF-TB implementation.
Box 1
Highlights from country case studies on MAF-TB adaptation and implementation
Belarus
In Belarus, the National Tuberculosis Programme (NTP), in collaboration with the secretariat of the Country Coordinating Mechanism of the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) and with the support of the MoH, initiated a baseline assessment using the MAF-TB checklist.
The baseline assessment recommended the establishment of a working group to develop a mechanism for the timely revision, adaptation and alignment of national protocols and strategic documents to the WHO guidelines, roadmaps and frameworks, and their timely implementation at national level. This recommendation is being implemented with support from the WHO Regional Office for Europe and the WHO Country Office for Belarus. Lessons learned from this experience will also help other countries in the region in their efforts to operationalize WHO guidelines.
Ukraine
In Ukraine, the results of the MAF-TB baseline assessment were presented and endorsed in the meeting of the National Council on Tuberculosis and HIV/AIDS in June 2021. One of the assessment recommendations was the development of a national roadmap for 2021–2023, for strengthening multisectoral collaboration and accountability mechanisms. This process will be coordinated jointly by the Secretariat of the National Council, MoH, NTP and a national group on advocacy, communication and social mobilization. A hearing of the Parliamentary Health Committee supported development of the national roadmap and requested the President Administration to organize an annual high-level review to track progress towards national targets and commitments to end TB.
To facilitate a joint vision on multisectoral coordination and accountability in the response to TB, national multistakeholder dialogue with TB-affected communities at the heart of the process and participation of relevant governmental ministries and bodies, and stakeholders beyond the health sector, is planned for November 2021.
Kenya
In Kenya, the process of MAF-TB adaptation and implementation is led by a national secretariat that includes representation from the NTP, WHO and the Stop TB Partnership-Kenya, with engagement of TB survivors (under their national network of champions) and other implementing partners.
In 2020, Kenya established a MAF-TB technical and coordinating committee. This developed a concise concept note with a roadmap, conducted a baseline assessment and mapped out relevant sectors and stakeholders. Several sectors were engaged (e.g. the ministries of Health, Education, Sports, Transport, Judiciary, Finance, Home Affairs and Foreign Affairs) in an analysis of strengths, weaknesses, opportunities and threats (SWOT), as the basis for definition of approaches and actions to be taken by stakeholders to ensure a multisectoral TB response. Subsequently, the development of a national MAF-TB document was initiated, with technical and financial support from the WHO Country Office in Kenya and the African Regional Office (AFRO), and in collaboration with partners and various sectors. This will culminate in a comprehensive framework that is scheduled for finalization and endorsement by the end of 2021.
Russian Federation
In the Russian Federation, a set of multisectoral measures at a high political level (including a high-level coordination mechanism) has achieved significant success in TB burden reduction. The country reached the 2020 milestones of the End TB Strategy for reduction of TB incidence and TB mortality and, for the first time in 22 years, left the list of high TB burden countries. The NTP of the Russian Federation has targets and commitments that align with the WHO End TB Strategy, and there is engagement of different sectors beyond the MoH (e.g. the penitentiary sector, labour, social protection, science, education, and industry and trade). The programme includes objectives for each of the sectors, with performance indicators set and the budget assigned. Monitoring, review and reporting is provided on a quarterly and annual basis. The overall supervision and coordination is provided by the government and prime minister, with regular reporting to the president.
Box 2
Multisectoral action to implement social protection for people affected by TB: examples of strategies supported by UN agencies
Multisectoral action and accountability to address the broader social and economic determinants and consequences of TB and achieve the End TB Strategy targets is taking place in several countries, with support from UN agencies and in close collaboration
with national governments and partners.
In Madagascar, the WFP is working with the NTP to provide nutrition support and counselling to malnourished TB patients. In 2020, WFP supported the development of a national integrated TB and HIV social and behaviour change communication
strategy, including nutrition-related behaviour change interventions.
In Djibouti, to mitigate the socioeconomic impact of the COVID-19 pandemic, WFP is complementing the national social protection programme (Programme National de Solidarité Famille, PNSF) with a cash transfer programme for the most vulnerable households affected by HIV and TB. In addition, WFP strongly advocates that national counterparts include these households into the PNSF. WFP, with the support of two local nongovernmental organizations (Le Réseau and Solidarité Féminine), and in close collaboration with the MoH and Ministry of Social Affairs and Solidarity (MASS), leads the implementation of this programme, which delivers cash to HIV and TB affected households for 9 months. To reduce barriers related to stigma and discrimination, beneficiaries are also enrolled in the national social registry managed by MASS, in the same way as other PNSF beneficiaries. Once enrolled in PNSF, beneficiaries are automatically eligible for health insurance under the Programme d'Assistance Sociale de Santé (PASS).
In India, the ILO is supporting implementation of the World of Work Programme. This programme aims to strengthen the integrated policy framework for TB and HIV/AIDS at the workplace, to secure employment and assure that workers with TB and HIV can continue medical treatment without discrimination in the workplace. It is implemented in collaboration with the Ministry of Health and Family Welfare, Ministry of Labor and Employment, civil society organizations, enterprises in the public and private sector, employers’ and workers’ organizations, and various development partners, such as the United States Agency for International Development (USAID), Joint United Nations Programme on HIV and AIDS (UNAIDS) and WHO. As a result of this multisectoral collaboration, a national integrated policy framework on addressing TB and HIV in the world of work was developed. Furthermore, in 2019, a “Statement of Commitment of Indian Employers’ organizations on addressing TB and HIV in the world of work” was jointly issued by public and private enterprises.
Fig. 1 MAF-TB essential components in place globally and in high TB burden countries (%)
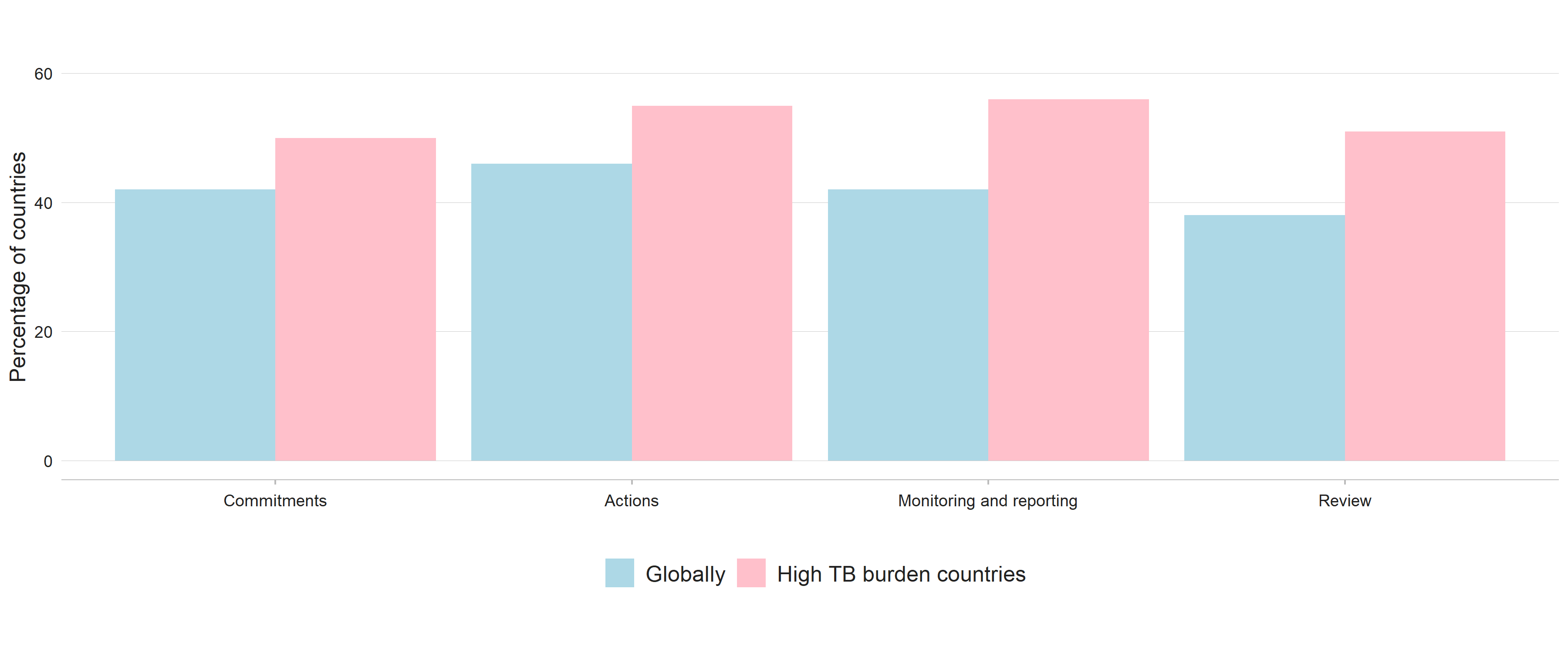
Table 1 Status of core elements of multisectoral accountability in 2021 for 30 high TB burden countries, WHO regions and globally
| High TB burden countries and WHO regions | Number of countries and territories | Annual national TB report publicly available | National multisectoral and multistakeholder accountability and review mechanism, under high-level leadership available | Engagement of civil society and affected communities in the multisectoral accountability and review mechanism |
|---|---|---|---|---|
| High TB burden countries | 30 | 29 (97%) | 19 (63%) | 15 (50%) |
| Africa | 47 | 43 (92%) | 31 (66%) | 29 (62%) |
| Americas | 45 | 24 (53%) | 22 (49%) | 11 (24%) |
| Eastern Mediterranean | 22 | 18 (82%) | 14 (64%) | 8 (36%) |
| Europe | 54 | 34 (63%) | 26 (48%) | 17 (32%) |
| South-East Asia | 11 | 10 (91%) | 10 (91%) | 6 (55%) |
| Western Pacific | 36 | 28 (78%) | 22 (61%) | 16 (44%) |
| Total | 215 | 157 (73%) | 125 (58%) | 87 (41%) |
TB: tuberculosis; WHO: World Health Organization.
References
- Villa S, Kasaeva T, Raviglione MC. A multisectoral approach to tuberculosis control and elimination in the era of the United Nations Sustainable Development Goals. In: Migliori GB & Raviglione MC (eds.), Essential tuberculosis. Cham, Springer. 2021 (https://doi.org/10.1007/978-3-030-66703-0_38).
- Resolution 73/3: Political declaration of the high-level meeting of the General Assembly on the fight against tuberculosis. New York: United Nations General Assembly; 2018 (https://www.un.org/en/ga/search/view_doc.asp?symbol=A/RES/73/3).
- Multisectoral accountability framework to accelerate progress to end tuberculosis by 2030. Geneva: World Health Organization; 2019 (https://covid.comesa.int/tb/WHO_Multisectoral_Framework_web.pdf).
- Overview: progress towards achieving global tuberculosis targets and implementation of the UN political declaration on tuberculosis. Geneva: World Health Organization; 2020 (https://covid.comesa.int/publications/m/item/overview-progress-towards-achieving-global-tuberculosis-targets-and-implementation-of-the-un-political-declaration-on-tuberculosis).
- About SPARKS Conference [website]. Stockholm: Karolinska Institutet; 2020 (https://sparksnetwork.ki.se/about-sparks-conference/).
- WHO multisectoral accountability framework for TB (MAF-TB): baseline assessment checklist for country use in pursuing a national MAF-TB. Geneva: World Health Organization; 2020 (https://covid.comesa.int/tb/publications/WHO_MAFTB_Checklist_Form-Final.pdf).
- WHO consolidated guidelines on drug-resistant tuberculosis treatment. Geneva: World Health Organization; 2019 (https://apps.who.int/iris/bitstream/handle/10665/311389/9789241550529-eng.pdf?ua=1).
