
6.1 Universal health coverage
The tuberculosis (TB) epidemic is strongly influenced by social and economic development, health-related risk factors (e.g. undernutrition, diabetes, HIV infection, alcohol use disorders and smoking), and geographic and financial access to health care (1–6).
Achieving global targets for reductions in TB disease burden and improved access to TB prevention, diagnosis and treatment services requires progress towards universal health coverage (UHC), combined with action to address health-related risk factors and the broader social and economic determinants and consequences of TB (7).
For example, the World Health Organization (WHO) End TB Strategy target to reduce the number of TB deaths by 75% between 2015 and 2025 is only feasible if, by 2025, everyone who develops TB disease can access high-quality treatment, such that the case fatality ratio (CFR; the percentage of people who develop TB disease that die from it) can be reduced to about 6.5%. This is a level already achieved in high-income countries. In addition, the End TB Strategy target to reduce TB incidence by 80% between 2015 and 2030 is only feasible if, by 2025, the annual decline in TB incidence can be accelerated to 10% per year, a rate of reduction previously documented only in the context of progress towards UHC and socioeconomic development.
All countries have committed to the End TB Strategy targets through their adoption of the End TB Strategy at the World Health Assembly in 2014, and to achieving UHC by 2030 through their adoption of the United Nations (UN) Sustainable Development Goals (SDGs). UHC, social protection and action on TB determinants are part of Pillar 2 of the End TB Strategy and SDG targets and indicators.
The definition of UHC is that everyone can obtain the health services they need without suffering financial hardship (8). Target 3.8 of the SDGs is to achieve UHC by 2030, a commitment that was reaffirmed at a UN high-level meeting in 2019 alongside a new target that an additional 1 billion people have access to quality essential health services by 2023 (9, 10). Two indicators are being used to monitor progress: a service coverage index (SCI) and an indicator of financial protection (Box 6.1.1).
Box 6.1.1
The two SDG indicators for UHC
The first SDG indicator for UHC is the coverage of essential health services (Indicator 3.8.1). This is measured using a service coverage index (SCI). The SCI has values from 0 to 100 and is based on 16 tracer indicators, one of which is TB treatment.
The second indicator is the proportion of the population with large household expenditures on health as a share of total household expenditure or income (Indicator 3.8.2). Two thresholds (10% and 25%) are used to define “large”. When household out-of-pocket expenditures on health surpass these thresholds, the expenditures are classified as “catastrophic” because they may adversely affect a household’s ability to pay for other basic needs.
Both SDG indicators are for the general population. Health expenditures are defined as direct expenditures on medical care, and the denominator includes many people who had no contact with the health system and thus had zero expenditures on health. Although these people did not experience financial hardship through direct expenditures on health care, they may nonetheless have faced financial barriers to accessing health services that they needed.
Indicator 3.8.2 cannot and should not be compared with the End TB Strategy indicator that is defined as the percentage of TB patients and their households facing catastrophic costs due to TB disease (Section 6.2). The TB-specific indicator includes not only direct medical payments for diagnosis and treatment, but also direct non-medical payments (e.g. transportation and lodging) and indirect costs (e.g. lost income). It is also restricted to a specific population: diagnosed TB patients who are users of health services that are part of national TB programme (NTP) networks.
Data for the SCI are currently available for 2000–2017 (Fig. 6.1.1). Globally, the SCI increased steadily in this period, from 45 (out of 100) in 2000 to 66 in 2017. Improvements were made in all WHO regions (especially the Western Pacific Region) and all World Bank income groups. In both 2000 and 2017, low-income and lower-middle-income countries had the lowest SCI values; however, they also had the fastest rate of increase in the SCI. There was little change over time in high-income countries. There is a great deal of variation among countries; in 2017, the highest values were in high-income countries in Asia, Europe and North America, whereas the lowest values were predominantly in countries in the WHO African Region (Fig. 6.1.2).
In contrast to improvements in the SCI, the level of financial protection for expenditures on health has worsened. Globally, the proportion of the general population facing catastrophic expenditures on health (using a threshold of >10% annual household income or expenditure) rose from 9.4% in 2010 to 12.7% (927 million people) in 2015 (11). National values are available for different years and there is more geographical variability compared with the SCI, including within regions (Fig. 6.1.3).
The distribution of the two UHC indicators in the 30 high TB burden countries and three global TB watchlist countries shows that, in general, values improve with income level, especially for the SCI (Fig. 6.1.4). Nonetheless, the risk of catastrophic health expenditures is high in several middle-income countries, including Bangladesh, Brazil, Cambodia, China, India, Myanmar and Nigeria. Thailand stands out as a high TB burden country with both a high SCI (80) and a high level of financial protection (2% of households facing catastrophic health expenditures). A UHC scheme was established in 2002, supported by domestic funding and a strong primary health care system (12).
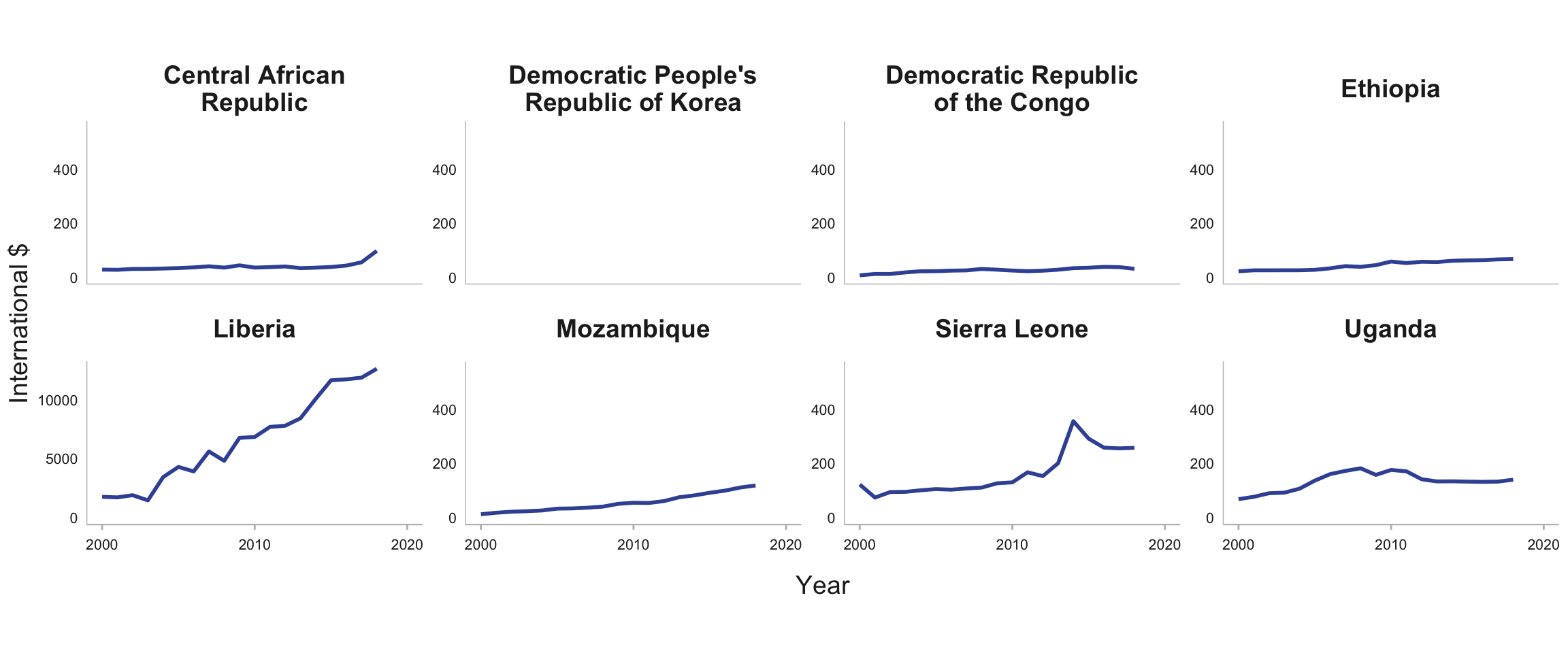
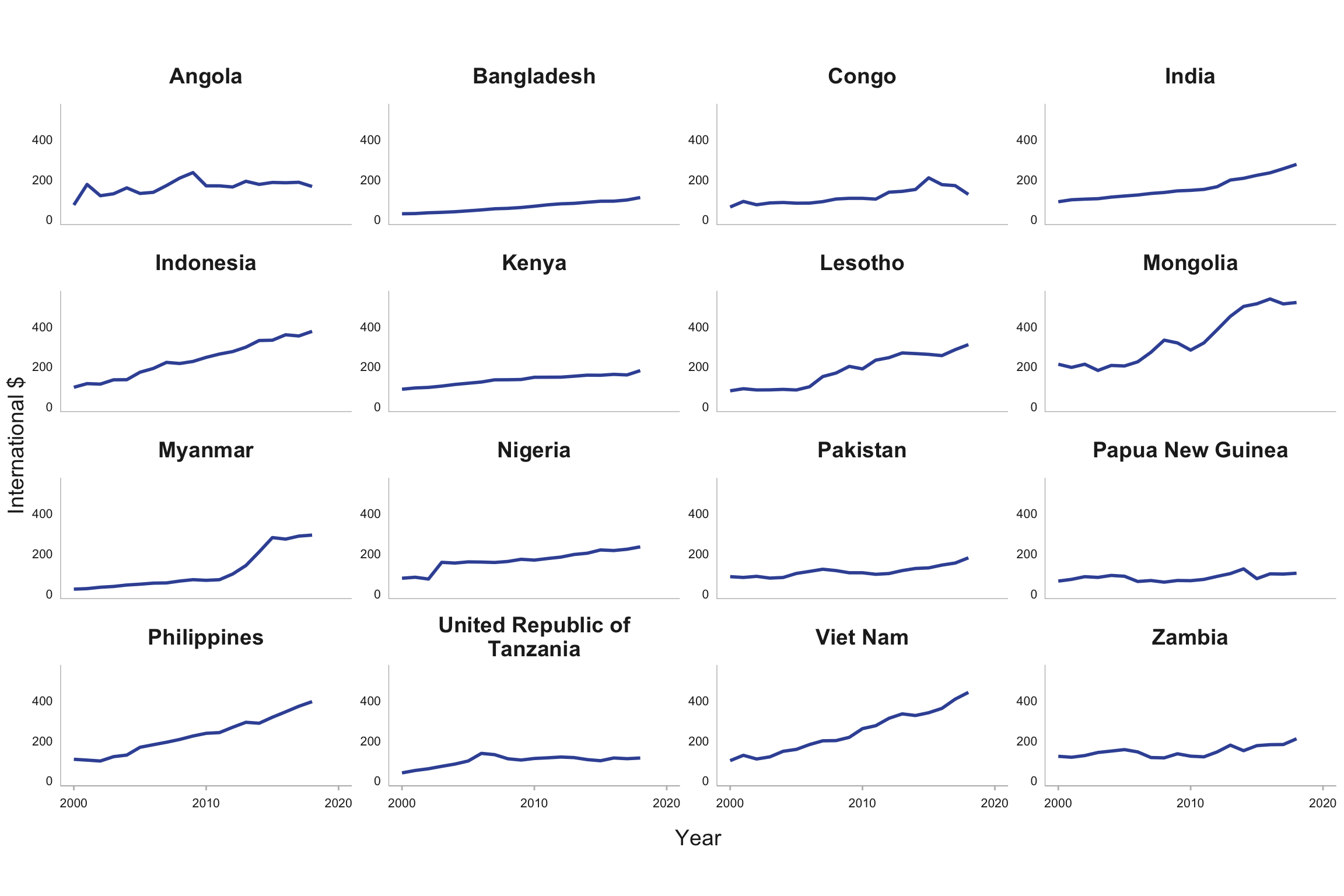
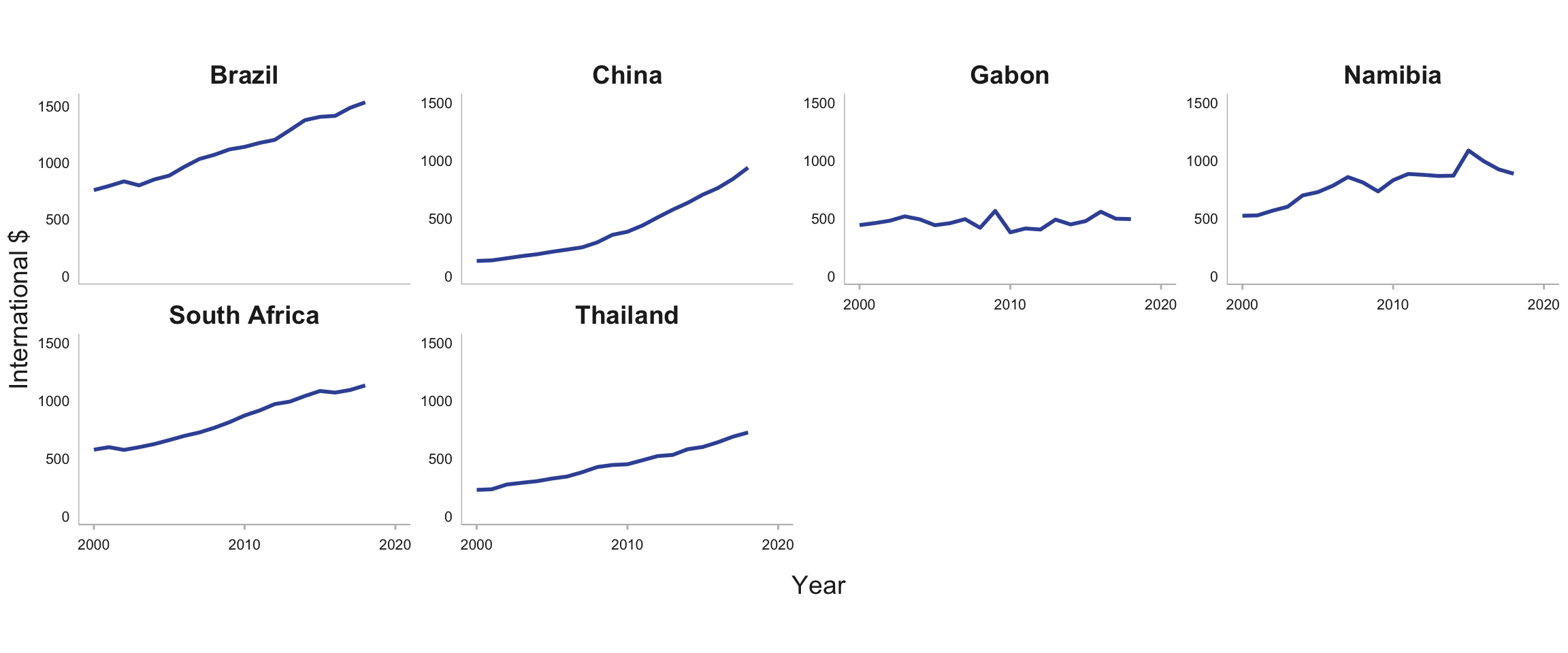
To achieve UHC, substantial increases in investment in health are critical. From 2000 to 2017 there was a striking increase in health expenditure (from all sources) per capita in a few high TB burden countries, especially the upper-middle-income countries of Brazil, China, South Africa and Thailand (Fig. 6.1.5). A steady upward trend was evident in India, Indonesia, Liberia, Mongolia, the Philippines and Viet Nam, and there was a noticeable rise from 2012 to 2017 in Myanmar. Elsewhere, however, levels of spending have been relatively stable, and at generally much lower levels.
Although data post-2017 are not yet available, the COVID-19 pandemic is likely to have caused progress towards UHC to stall or reverse in 2020 and 2021 in many countries.
Further country-specific data for the two SDG indicators for UHC are available in the Global tuberculosis report app and online country profiles.
Fig. 6.1.1 Trends in the UHC service coverage index in WHO regions and World Bank income groups, 2000–2017
(a) By region
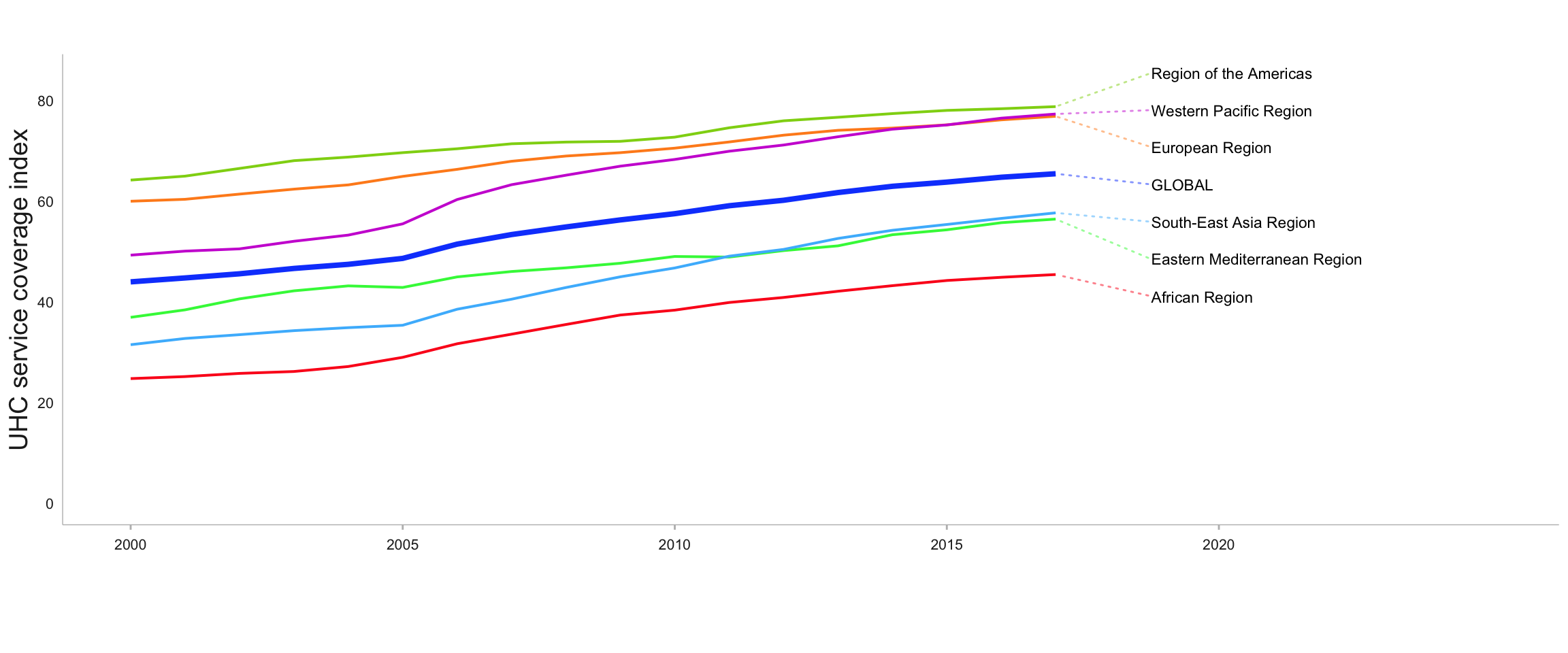
(b) By income group
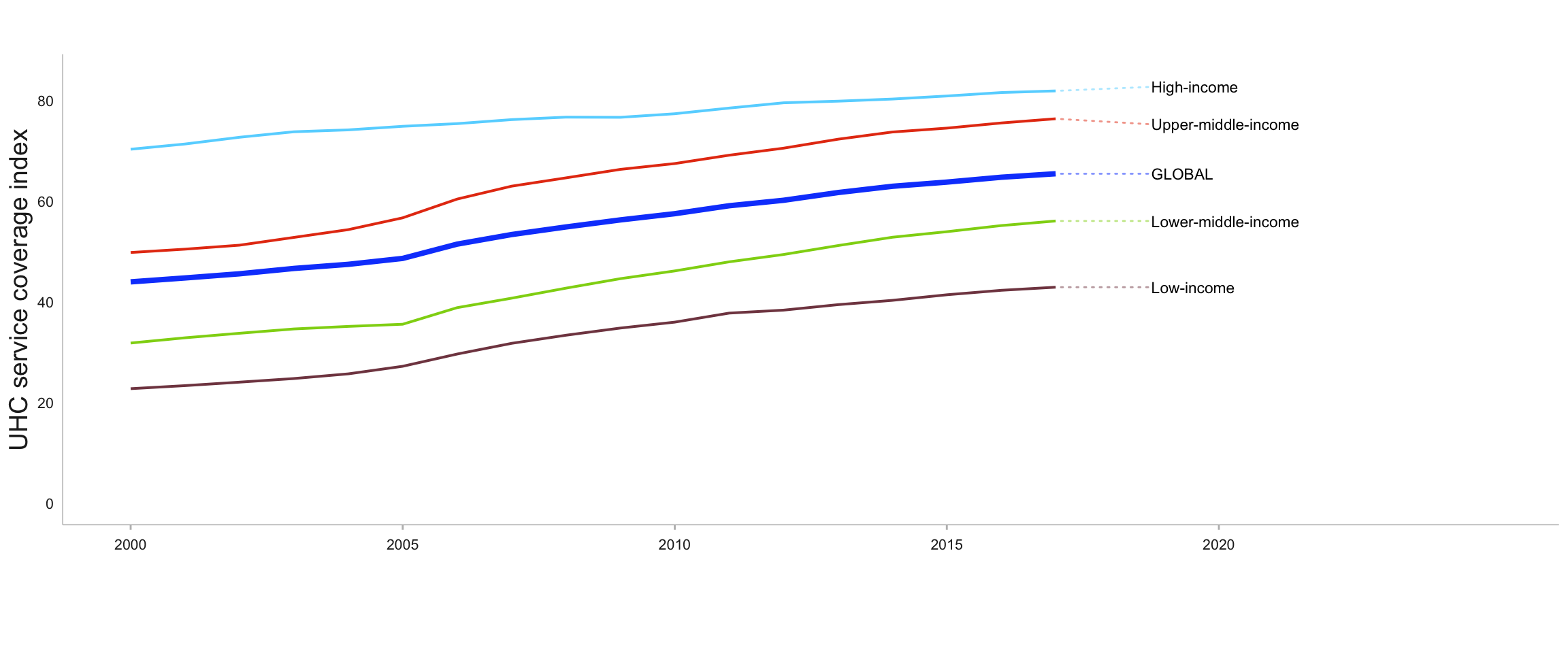
Fig. 6.1.2 UHC service coverage index by country, 2017
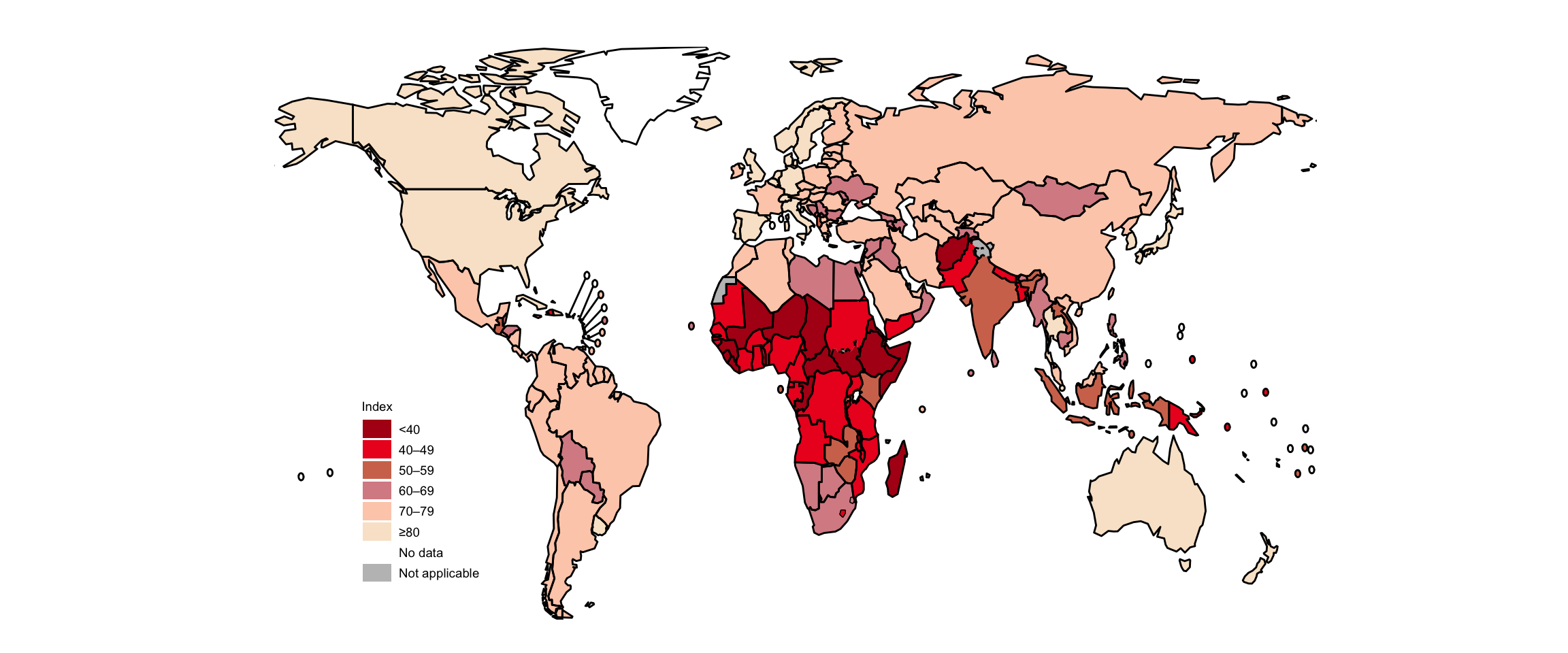
Fig. 6.1.3 Percentage of the general population facing catastrophic health expenditure,a latest available year of datab
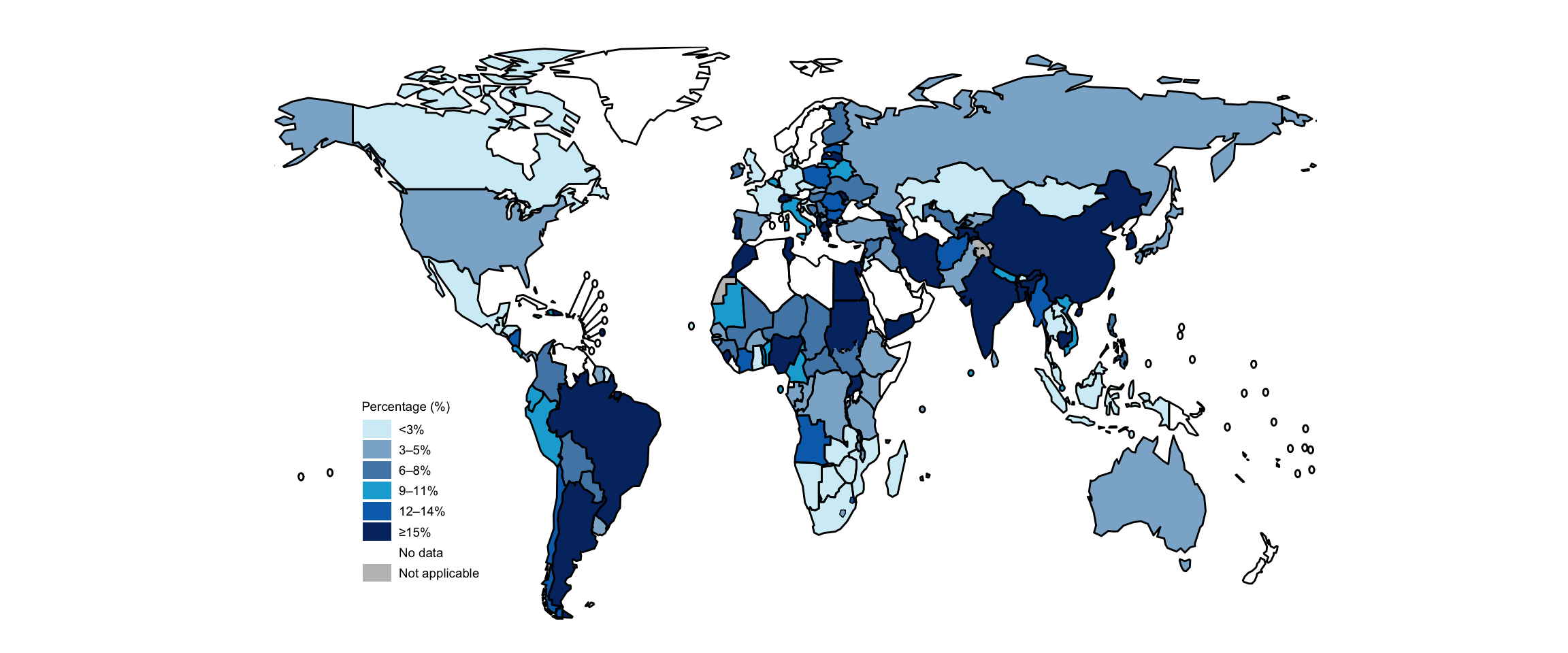
b The latest available year ranges from 2000 to 2018.
Source: WHO Universal Health Coverage data portal (http://apps.who.int/gho/portal/uhc-overview.jsp)
Fig. 6.1.4 UHC service coverage index (SDG 3.8.1)a and percentage of the general population facing catastrophic health expenditures (SDG 3.8.2),b 30 high TB burden countries and three global TB watchlist countries,c stratified by income groupd
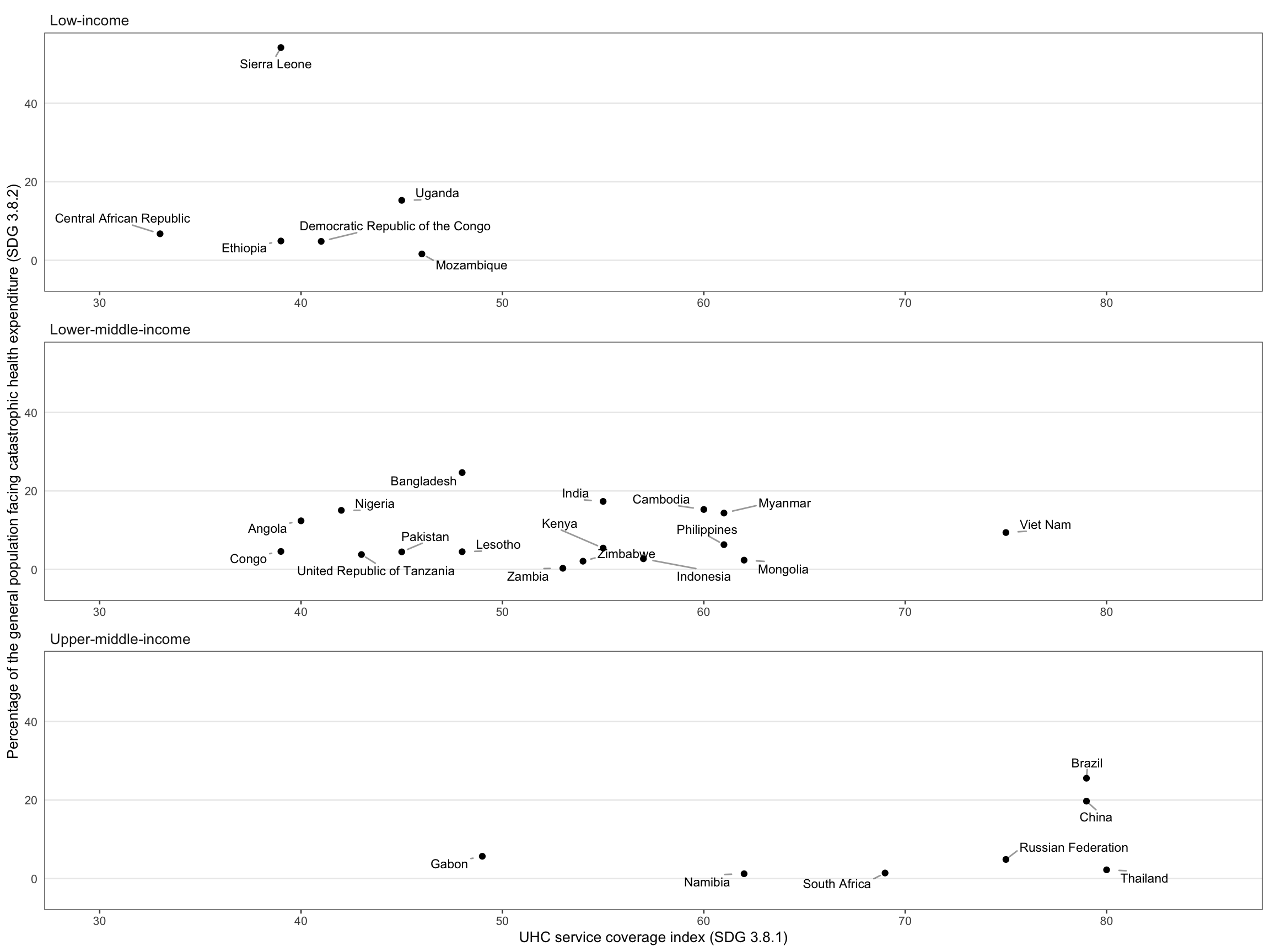
b Defined as ≥10% of total household consumption or income. The latest available year ranges from 2007 to 2018 for the 30 high TB burden countries.
c The three global TB watchlist countries are Cambodia, Russian Federation and Zimbabwe.
d As per the 2021 World Bank classification.
Source: WHO Universal Health Coverage data portal (http://apps.who.int/gho/portal/uhc-financial-protection-v3.jsp)
Fig. 6.1.5 Current health expenditure per capita, 30 high TB burden countries, 2000–2018
(a) Low-income countries
(b) Lower-middle-income countries
(c) Upper-middle-income countries
References
- Grange JM, Gandy M, Farmer P, Zumla A. Historical declines in tuberculosis: nature, nurture and the biosocial model. Int J Tuberc Lung Dis. 2001;5(3):208–12 (https://www.ncbi.nlm.nih.gov/pubmed/11326817).
- Styblo K, Meijer J, Sutherland I. [The transmission of tubercle bacilli: its trend in a human population]. Bull World Health Organ. 1969;41(1):137–78 (https://www.ncbi.nlm.nih.gov/pubmed/5309081).
- Lienhardt C, Glaziou P, Uplekar M, Lönnroth K, Getahun H, Raviglione M. Global tuberculosis control: lessons learnt and future prospects. Nat Rev Microbiol. 2012;10(6):407 (https://www.ncbi.nlm.nih.gov/pubmed/22580364).
- Lönnroth K, Castro KG, Chakaya JM, Chauhan LS, Floyd K, Glaziou P et al. Tuberculosis control and elimination 2010–50: cure, care, and social development. Lancet. 2010;375(9728):1814–29 (https://www.ncbi.nlm.nih.gov/pubmed/20488524).
- Lönnroth K, Jaramillo E, Williams B, Dye C, Raviglione M. Tuberculosis: the role of risk factors and social determinants. In: Blas E & Kurup A (eds.), Equity, social determinants and public health programmes. 2010 (https://apps.who.int/iris/bitstream/handle/10665/44289/9789241563970_eng.pdf;jsessionid=067BC8BA3F7A5366C05BE34404F9D8F6?sequence=1).
- Lönnroth K, Jaramillo E, Williams BG, Dye C, Raviglione M. Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc Sci Med. 2009;68(12):2240–6 (https://www.ncbi.nlm.nih.gov/pubmed/19394122).
- Floyd K, Glaziou P, Houben R, Sumner T, White RG, Raviglione M. Global tuberculosis targets and milestones set for 2016–2035: definition and rationale. Int J Tuberc Lung Dis. 2018;22(7):723–30 (https://www.ncbi.nlm.nih.gov/pubmed/29914597).
- World Health Organization/World Bank. Tracking universal health coverage: 2017 global monitoring report. Geneva: World Health Organization; 2017 (https://apps.who.int/iris/bitstream/handle/10665/259817/9789241513555-eng.pdf).
- Sustainable development goals [website]. New York: United Nations (https://sustainabledevelopment.un.org/topics/sustainabledevelopmentgoals).
- United Nations General Assembly. Resolution 74/2: Political declaration of the high-level meeting of the General Assembly on universal health coverage. United Nations; 2019 (https://undocs.org/en/A/RES/74/2).
- World Health Organization/World Bank. Global monitoring report on financial protection in health 2019. Geneva: World Health Organization; 2020 (https://apps.who.int/iris/bitstream/handle/10665/331748/9789240003958-eng.pdf).
- Tangcharoensathien V, Witthayapipopsakul W, Panichkriangkrai W, Patcharanarumol W, Mills A. Health systems development in Thailand: a solid platform for successful implementation of universal health coverage. Lancet. 2018;391(10126):1205–23 ( https://pubmed.ncbi.nlm.nih.gov/29397200/) .
