
1.1 TB incidence
Box 1.1.1 summarizes the methods used to produce estimates of TB incidence between 2010 and 2019, and the new methods that were needed to produce estimates for 2020–2022. Estimation of TB incidence during the COVID-19 pandemic and its aftermath is much more difficult than previously. The new methods were extensively reviewed in 2021 and 2022 but rely heavily on country and region-specific dynamic models for low and middle-income countries that experienced major COVID-related disruptions to TB diagnosis and treatment, in the absence of reliable direct measurements of disease burden from national disease surveillance systems or population-based surveys.
An estimated global total of 10.6 million people (95% uncertainty interval [UI]: 9.9–11.4 million) fell ill with TB in 2022, equivalent to 133 incident cases (95% UI: 124–143) per 100 000 population (Table 1.1.1). Among all incident TB cases, 6.3% were among people living with HIV. Most TB cases in 2022 were in the WHO regions of South-East Asia (46%), Africa (23%) and the Western Pacific (18%), with smaller shares in the Eastern Mediterranean (8.1%), the Americas (3.1%) and Europe (2.2%).
| Region or country group | Population | Best estimate | Low | High | Best estimate | Low | High | Best estimate | Low | High | Best estimate | Low | High |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| African Region | 1 190 000 | 2 480 | 2 190 | 2 780 | 461 | 395 | 533 | 208 | 184 | 233 | 39 | 33 | 45 |
| Region of the Americas | 1 040 000 | 325 | 300 | 351 | 41 | 37 | 45 | 31 | 29 | 34 | 3.9 | 3.5 | 4.4 |
| South-East Asia Region | 2 070 000 | 4 850 | 4 380 | 5 350 | 99 | 80 | 119 | 234 | 211 | 258 | 4.8 | 3.9 | 5.8 |
| European Region | 931 000 | 229 | 196 | 263 | 28 | 20 | 37 | 25 | 21 | 28 | 3.0 | 2.2 | 4.0 |
| Eastern Mediterranean Region | 780 000 | 856 | 674 | 1 060 | 4.2 | 3.3 | 5.2 | 110 | 86 | 136 | 0.54 | 0.42 | 0.67 |
| Western Pacific Region | 1 940 000 | 1 860 | 1 450 | 2 330 | 38 | 27 | 50 | 96 | 75 | 120 | 1.9 | 1.4 | 2.6 |
| High TB burden countries | 4 910 000 | 9 200 | 8 470 | 9 950 | 536 | 467 | 609 | 187 | 173 | 203 | 11 | 9.5 | 12 |
| Global | 7 950 000 | 10 600 | 9 870 | 11 400 | 671 | 600 | 746 | 133 | 124 | 143 | 8.4 | 7.5 | 9.4 |
The estimated 10.6 million people (95% UI: 9.9–11.4 million) who fell ill with TB worldwide in 2022 is an increase from 10.3 million in 2021 (95% UI: 9.6–11 million) and 10.0 million (95% UI: 9.4–10.7 million) in 2020, continuing the reversal of the downward trend that had been sustained for many years up to 2020 (Fig. 1.1.1a). Similarly, the TB incidence rate (new cases per 100 000 population per year) is estimated to have increased by 1.9% between both 2020–2021 and 2021–2022 (Fig. 1.1.1b).
Two consecutive years of global increases in TB incidence (in 2021 and 2022) mean that in 2022, the TB incidence rate reverted back to the level of 2019 (Fig. 1.1.1b). Globally, the net reduction in the TB incidence rate from 2015 to 2022 was 8.7%, far from the WHO End TB Strategy milestone of a 50% reduction by 2025 (1, 2).
These estimated increases in TB incidence in 2021 and 2022 are the consequence of disruptions to TB diagnosis and treatment during the COVID-19 pandemic, when the reported number of people newly diagnosed with TB fell from 7.1 million in 2019 to 5.8 million in 2020 and 6.4 million in 2021 (Section 2.1). While the most immediate impact of an increase in the number of people with undiagnosed and untreated TB is on TB mortality (Section 1.2), it also results in increased transmission of TB and then, with a lag time (given the time from infection to progression to TB disease ranges among individuals from months to years), an increase in the number of people developing TB disease. Similarly, the most immediate impact of the big global recovery in the reported number of people newly diagnosed with TB in 2022 (Section 2.1) is on TB mortality. Reversing the global increase in TB incidence will take longer; previous projections suggest that it might occur in 2023 or 2024.
Of note, it was recognized that the impact of an increased number of people with undiagnosed and untreated TB on TB transmission could be partially offset by COVID-related restrictions. The dynamic models used to estimate TB incidence in countries that had large reductions in TB case notifications (relative to pre-pandemic trends) in 2020 and/or 2021 assumed a 50% reduction in transmission during severe restrictions (lockdowns).
In 2022, eight countries accounted for more than two thirds of global TB cases: India (27%), Indonesia (10%), China (7.1%), the Philippines (7.0%), Pakistan (5.7%), Nigeria (4.5%), Bangladesh (3.6%) and the Democratic Republic of the Congo (3.0%) (Fig. 1.1.2).

The severity of national TB epidemics, in terms of the number of incident TB cases per 100 000 population in 2022, varies widely among countries: from less than ten to more than 500 new and relapse cases per 100 000 population (Fig. 1.1.3).
Countries with the highest rates were mostly in the African Region. There were 57 countries with a low incidence of TB (<10 cases per 100 000 population per year), mostly in the WHO Region of the Americas and the European Region, plus a few countries in the WHO Eastern Mediterranean and Western Pacific regions.

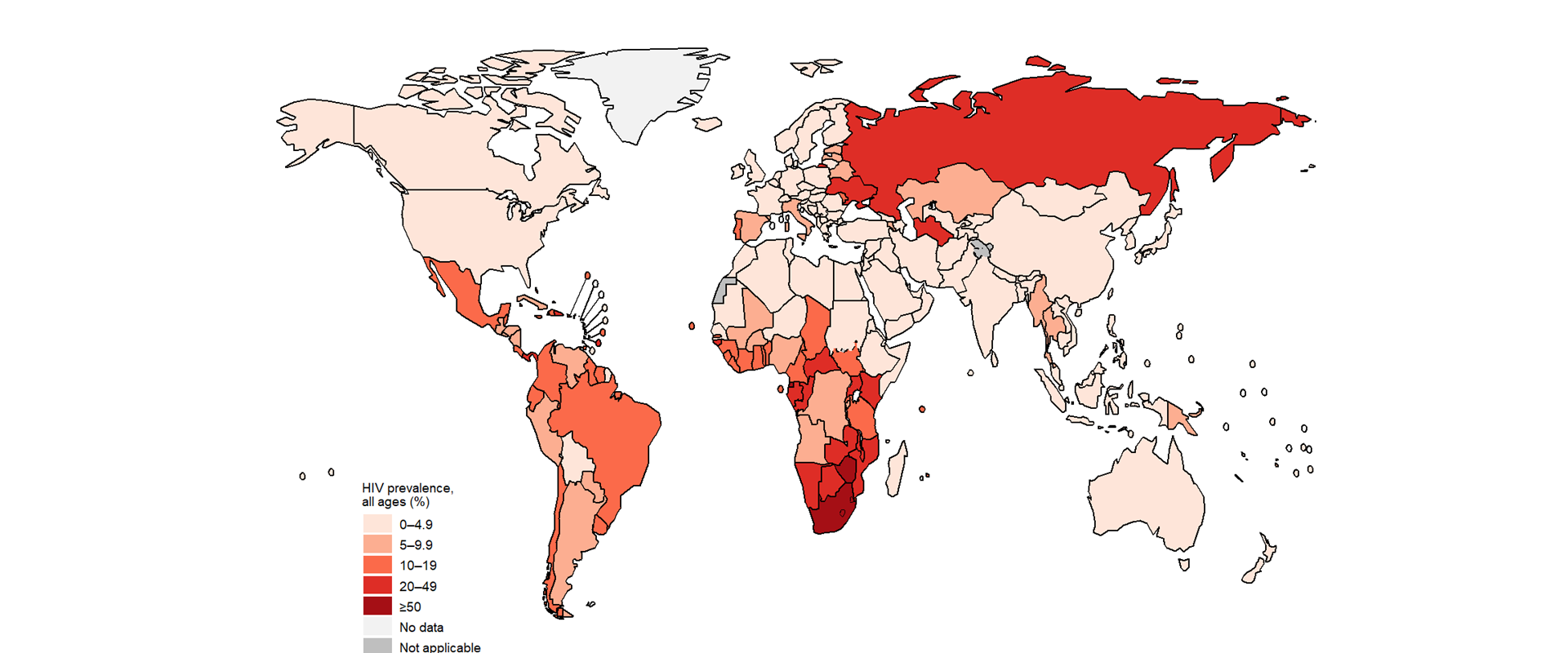
In 2022, the proportion of people with a new episode of TB (either new or relapse cases) who were coinfected with HIV was highest in countries in the WHO African Region, exceeding 50% in parts of southern Africa (Fig. 1.1.4).
TB can affect anyone, regardless of age or sex (Fig. 1.1.5). The highest burden is in adult men (aged ≥15 years), with an estimated 5.8 million cases (95% UI: 5.4–6.2 million) in 2022, equivalent to 55% of the estimated total; by comparison, there were an estimated 3.5 million cases (95% UI: 3.3–3.8 million) among adult women (aged ≥15 years), equivalent to 33% of the estimated total, and 1.3 million (95% UI: 1.2–1.3 million) cases among children (aged 0–14 years), equivalent to 12% of the estimated total. Case notifications of people newly diagnosed with TB in 2022 were 70% of the estimated TB incidence overall but this varied by age and sex: 72% for adult men, 75% for adult women and 49% for children aged 0–14 years. Among children aged <5 years, the figure was only 42%.
Regional estimates of the distribution of incident TB cases, disaggregated by age and sex and compared with case notifications, are shown in Fig. 1.1.6.
Regional trends in TB incidence vary and progress in relation to the 2025 milestone of the End TB Strategy is mixed (Fig. 1.1.7).
The TB incidence rate increased for the second consecutive year in three of the six WHO regions, reflecting the estimated impact of shortfalls in TB case detection in 2020 and incomplete recovery in 2021 and 2022. An upward trend between 2020 and 2021 was reversed in 2022 in two regions: the Eastern Mediterranean Region (back to the level of 2020) and the European Region (almost back to the level of 2020). In the African Region, the decline that has been sustained for many years was maintained in 2022, consistent with evidence that disruptions related to the COVID-19 pandemic had little impact on the number of people diagnosed and officially notified with TB in either 2020 or 2021 (Section 2.1).
The biggest reduction compared with the baseline year of 2015 has been in the European Region, with a net reduction of 25% by 2022. A similar reduction has been achieved in the African Region, with a 23% decline by 2022. The net decline by 2022 compared with 2015 was relatively small in three of the remaining WHO regions: the Eastern Mediterranean Region (7.4%), South-East Asia (6.6%) and the Western Pacific (3.7%). The most concerning trend is in the Region of the Americas, where there was a net increase of 14% between 2015 and 2022.
Progress in reducing the TB incidence rate at country level is highly variable (Fig. 1.1.8). A total of 83 countries, mostly in the WHO African and European regions, achieved estimated reductions of at least 20% between 2015 and 2022, thus reaching or surpassing the first (2020) milestone of the End TB Strategy. A total of 21 countries are estimated to have achieved reductions of at least 50% between 2015 and 2022, including one high TB burden country (South Africa). At the other extreme, there are countries where TB incidence in 2022 was more than 5% higher than in 2015. These countries are most noticeably in the Region of the Americas but also include four high TB burden countries in Asia: Indonesia, Mongolia, Myanmar and the Philippines.

Trends in the TB incidence rate in the 30 high TB burden countries are also highly variable (Fig. 1.1.9).
In 2021 and 2022, the estimated TB incidence rate increased in two of the three global TB watchlist countries, while the Russian Federation is close to reaching the 2025 milestone of the End TB Strategy (Fig. 1.1.10).
Box 1.1.1
Methods used by WHO to estimate TB incidence
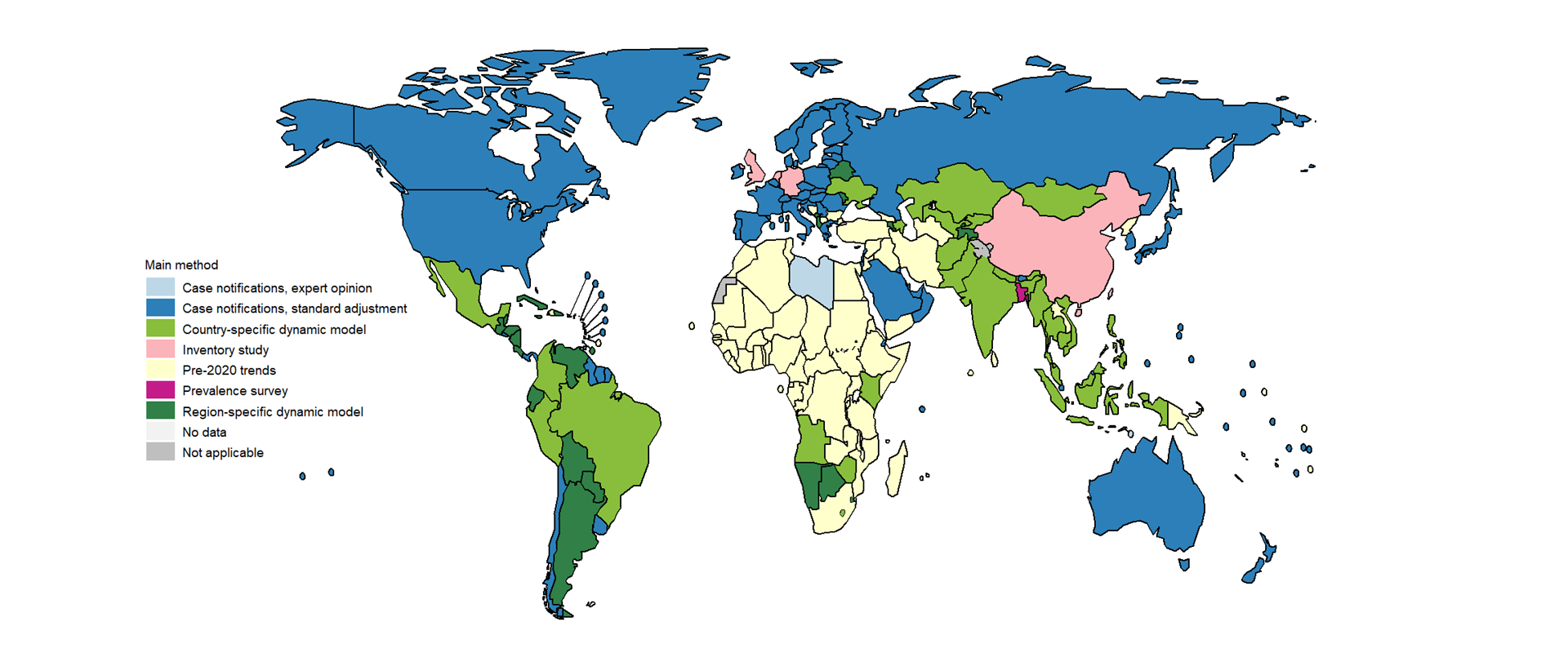
The main methods used by WHO to estimate TB incidence at country level in the periods 2010–2019 and 2020–2022 are shown in Fig. 1.1.11 and Fig. 1.1.12. These methods adhere to global guidelines for accurate and transparent reporting of health estimates (3) and are described in detail in a technical appendix.
Methods used by WHO to estimate TB incidence for 2010–2019 included:
results from national TB prevalence surveys combined with estimates of the duration of disease and assumptions about the trend in TB incidence for countries with a single survey, used for 28 countries with 39% of the global number of incident TB cases in 2019;
results from a national TB prevalence survey combined with a country-specific dynamic model that was calibrated to survey data as well as other data (e.g. notifications, drug sales) and WHO TB mortality estimates. This was used for India, which had 27% of the global number of incident TB cases in 2019 (for further details, see Annex 5 and the technical appendix);
case notification data adjusted by a standard factor to account for underreporting, overdiagnosis and underdiagnosis, used for 139 countries (including most high-income countries and selected middle-income countries and areas) with about 6.0% of the global number of incident TB cases in 2019;
results from national inventory studies that measured the level of underreporting of detected TB cases, used for eight countries with about 17% of the global number of incident TB cases in 2019; and
case notification data combined with expert opinion about underreporting and underdiagnosis, used for 39 countries with 11% of the global number of incident TB cases in 2019.
Estimates of TB incidence in 2020, 2021 and 2022 were based on country-specific dynamic models for 25 countries with the biggest absolute reductions in TB notifications during the COVID-19 pandemic (excluding countries where reductions were consistent with pre-2020 trends), and either region-specific dynamic models (23 countries) or pre-2020 trends for other low and middle-income countries. Estimates for high-income countries were based on the same methods as those used up to 2019 i.e. notification data with a standard adjustment.
Estimates of TB incidence in 2020 and 2021 have been revised downwards for several countries, compared with those published in 2022, resulting in downward revisions to the global estimates. Further details are provided in Annex 5 of the main report.

Country-specific details are available in the Global tuberculosis report app and country profiles.
Note: All of the percentage reductions or increases referred to in the text of this webpage were calculated based on unrounded numbers, as opposed to the rounded numbers that appear in the interactive graphics.
References
Floyd K, Glaziou P, Houben R, Sumner T, White RG, Raviglione M. Global tuberculosis targets and milestones set for 2016-2035: definition and rationale. Int J Tuberc Lung Dis. 2018;22(7):723-30 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6005124/).
World Health Organization. Resolution WHA67.1. Global strategy and targets for tuberculosis prevention, care and control after 2015. Geneva: World Health Organization; 2014 (https://iris.who.int/handle/10665/162760).
Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) [website] (http://gather-statement.org/).
