Situation at a glance
Description of the situation
On 14 July 2022, the Ministry of Health (MoH) of the United Republic of Tanzania notified WHO of 13 cases of an undiagnosed disease, later diagnosed as leptospirosis. The first two cases presented to a Health Centre located in Ruangwa District, Lindi Region on 5 and 7 July, with symptoms of fever, bleeding from the nose, headache and general body weakness. Samples tested negative for Ebola virus disease, Marburg virus disease, Influenza, Crimean-Congo haemorrhagic fever, yellow fever, Chikungunya, West Nile virus and Rift Valley fever at the National Public Health Laboratory and the Tanzania Veterinary Laboratory Agency, and subsequently tested positive for leptospirosis at the Sokoine University of Agriculture reference laboratory.
As of 8 August, a total of 20 cases of leptospirosis and three deaths had been reported from two districts including Ruangwa (18 cases) and Kilwa (two cases) in Lindi Region (Figure 1). Of these, 15 cases have been laboratory-confirmed, including one death (case fatality rate 6.7%). Of the remaining five cases, three cases, including one death, tested negative for leptospirosis while samples were not taken for two cases, of which one died.
The cases ranged from 18 to 77 years of age (median age 45 years) and the majority (n=15; 75%) were between 31 and 60 years. Most of the cases (n=15, 75%) were males, who were farmers by occupation and were detected in a temporary camp for agricultural activities.
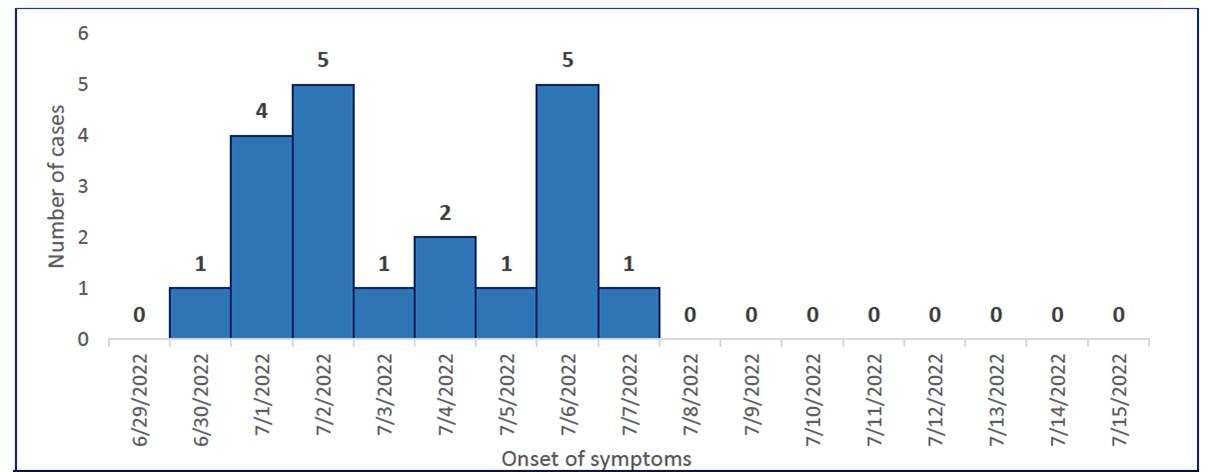
Cases who reported onset of symptoms from 30 June to 3 July were identified in the community during active case finding. The majority of cases reported onset of symptoms between 2 and 6 July, and the most recent cases reported onset of symptoms on 7 July. No new cases have been reported since 15 July (Figure 2). Field investigations and active case finding are ongoing to identify any new or missed cases.
Figure 1: Geographic distribution of suspected cases of leptospirosis in the United Republic of Tanzania, as of 15 July 2022

Figure 2: Suspected cases of leptospirosis by onset of symptoms, as of 15 July 2022
 Source: United Republic of Tanzania Ministry of Health.
Source: United Republic of Tanzania Ministry of Health.
Epidemiology
Leptospirosis is a zoonotic disease caused by the Leptospira genus of bacteria, and a worldwide public health problem attributed to climatic and environmental conditions. Humans become infected through contact with urine (or other body fluids, except saliva) from infected animals, such as rodents, dogs, pigs, cattle, horses, racoons, and wild animals, or contact with water, soil, or food contaminated with the urine of infected animals. Human-to-human transmission occurs only very rarely. The incubation period is usually 7–10 days, with a range of 2–30 days.
Clinical features of leptospirosis include fever, headache, myalgia (particularly in the calf muscle), conjunctival suffusion, jaundice, and general malaise. As these symptoms are similar to other infectious diseases, it is important to correctly diagnose early after the onset of symptoms to treat patients and prevent severe illness. Severe cases include renal and cardiac failure as well as pulmonary hemorrhages and can mimic other epidemic diseases of international importance.
Outbreaks of leptospirosis are rare, with a seasonal distribution, increasing with increased rainfall or higher temperature, and are usually caused by exposure to contaminated water, such as floodwaters or may be associated with changes in human behaviour, animal or sewage contamination of water, changes in animal reservoir density, or following natural disasters.
Public health response
- On 18 July, the MoH issued a press release notifying the outbreak and initiated coordination mechanisms at national and regional levels. A detailed national health sector response plan has been developed.
- The MoH, in collaboration with WHO, deployed a multidisciplinary rapid response team to the affected areas and response activities were implemented.
- Surveillance activities including epidemiological investigations and active case finding are ongoing. This includes enhanced surveillance for human and animal health.
- Training on leptospirosis including integrated disease surveillance and response was conducted for health care workers in Ruangwa district.
- Sensitization activities of health care workers on clinical presentation and infection prevention and control (IPC) are ongoing. Leptospirosis factsheets have been printed and distributed to all health care facilities in the affected areas.
- Additional samples have been collected from human, animal, and water sources for laboratory testing.
- Cases were provided with appropriate medical care. Medicines and medical equipment including personal protective equipment were provided to the region.
- Health education is being broadcasted through the local radio station delivering accurate health information to the community and answering their questions.
WHO risk assessment
WHO assesses the overall risk at the national level as moderate. Although the exact source of the outbreak remains unidentified, it is likely linked to farming activities. The affected areas attract farmers from other locations who make temporary settlements while farming and the area has a seasonal influx of farmers, inferring that many other people can be exposed to the same source of contamination and the number of cases may increase.
In addition, the affected areas have limited basic services including water supply, sanitation and hygiene, and health care services. It is therefore anticipated that IPC capacities at the community level would be weak. Moreover, the country’s capacity to respond to this outbreak might become overwhelmed, if the number of cases and affected areas increase in addition to other ongoing health threats. Leptospirosis has been previously reported in the United Republic of Tanzania (2014, in Kigoma Region) and is a recognized public health risk. However, the incidence in different regions is not well known and surveillance capacity is limited.
The risk of disease spread both at regional and global levels is considered Low.
WHO advice
The control of leptospirosis is complicated and will depend on the local conditions. Control can be achieved by controlling the disease reservoir. Preventive measures must be based on a knowledge of the groups at particular risk of infection and the local epidemiological factors. Prevention and control should be targeted at: (a) the infection source; (b) the route of transmission between the infection source and the human host; or (c) infection or disease in the human host.
Transmission can therefore be prevented by:
- wearing protective clothing (boots, gloves);
- covering skin lesions with waterproof dressings;
- washing or showering after exposure to urine splashes or contaminated soil or water;
- washing and cleaning wounds;
- developing an awareness of potential risks and methods of preventing or minimizing exposure, for instance by avoiding or preventing urine splashes and aerosols, avoiding touching ill or dead animals, fetuses, placentas, organs (kidneys, bladders) with bare hands, and, unless wearing gloves, avoiding assisting animals giving birth;
- strictly maintaining hygienic measures during care or handling all animals, including wearing gloves when handling the urine of dogs and other animals, washing hands afterward, and being aware that it is possible to be infected while nursing sick dogs or other animals;
- where feasible, disinfecting contaminated areas (scrubbing floors in stables, butcheries, abattoirs, etc.).
- providing clean drinking water;
- preventing access to or giving adequate warning of water bodies known or suspected to be contaminated (pools, ponds, rivers);
- introducing good herd management (avoiding communal pastures, buying certified leptospire-free stock);
- implementing standard safety procedures in laboratories.
When an outbreak occurs, both health care workers and the general public need to be rapidly informed of the situation and of the ways in which the disease may be prevented. Widespread community education can greatly assist in the identification of risk factors, the prevention of illness, and reducing the duration of illness and its severity through the early recognition of suspicious symptoms and self-referral for evaluation and treatment.
The general public should be provided with information on the clinical signs of leptospirosis, on the risk of exposure, and on the importance of seeking medical care as soon as possible as the disease responds to antibiotics. Information should also be given on methods of prevention, such as people should avoid drinking or submerging in water that may be contaminated, and not wash clothes in potentially contaminated water if any open wounds are present.
Health care providers should be given information to help them recognize a febrile illness, possibly due to leptospirosis, and on suitable treatments for the disease. Health care workers caring for patients with suspected or confirmed leptospirosis should apply standard and transmission-based IPC precautions. In addition, information on the symptoms of leptospirosis, risk factors, diagnostic testing and therapeutic strategies should be regularly disseminated to health care workers through various channels.
Surveillance activities including active case search should be reinforced in all affected areas and surroundings. The One Health approach should also be strengthened with surveillance activities reinforced not only with regard to human health but also animal and environmental health.
WHO does not recommend any restriction on travel or trade to the United Republic of Tanzania based on the current situation.
Further information
- World Health Organization Regional Office for Africa, Outbreaks and Emergencies Bulletin, Week 30: 18 to 24 July 2022. Available at: https://www.afro.who.int/countries/united-republic-of-tanzania/publication/outbreaks-and-emergencies-bulletin-week-30-18-24-july-2022 ·
- World Health Organization and International Leptospirosis Society. Human leptospirosis: guidance for diagnosis, surveillance and control Technical document. 9 August 2003. Available at: https://covid.comesa.int/publications/i/item/human-leptospirosis-guidance-for-diagnosis-surveillance-and-control.
- Leptospirosis. Organización Panamericana de la Salud PAHO. Available at: https://www.paho.org/es/temas/leptospirosis
- Centers for Disease Control and Prevention. Leptospirosis. 13 March 2019. Available at: https://www.cdc.gov/leptospirosis/index.html (link is external).
- World Health Organization. Water, sanitation and hygiene. Available at: https://covid.comesa.int/health-topics/water-sanitation-and-hygiene-wash.
Citable reference: World Health Organization (12 August 2022). Disease Outbreak News; Leptospirosis in the United Republic of Tanzania . Available at: https://covid.comesa.int/emergencies/disease-outbreak-news/item/2022-DON403
