In line with the COVID-19 Emergency Committee recommendations, WHO supported the government to conduct the COVID-19 Intra Action Review (IAR) from 11 to 14 August 2020, a comprehensive multi-sectoral review, to identify gaps and opportunities for learning and provide recommendations to improve the COVID-19 response.
The MoH has already conducted four meetings to monitor implementation of IAR recommendations in November 2020, February, April and August 2021. The fifth monitoring meeting was conducted from 15-18 February 2022 with a special focus on reviewing the response to the Omicron variant. Participants discussed the 11 IAR pillars: (1) command and coordination; (2) risk communication and community empowerment; (3) surveillance, rapid response teams and case investigation; (4) points of entry, international travel, and transport; (5) laboratory; (6) infection prevention and control; (7) case management; (8) operational and logistics support; (9) maintaining of essential health services and systems; (10) vaccination; and (11) public health and social measures. Participants also discussed the achievements of the health sector COVID-19 response plan indicators.
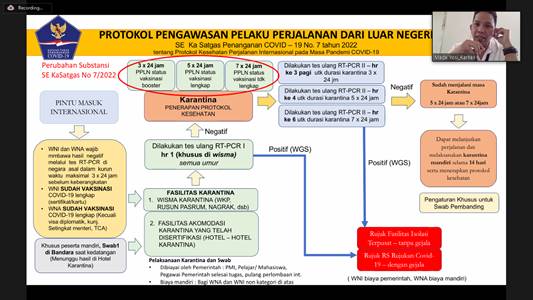
Fig. 1. Dr. I Made Yosi Purbadi Wirentana from the Ministry of Health presented an update on interventions related to the COVID-19 response at designated PoEs (Credit: Endang Wulandari/WHO)
Dr Maxi Rein Rondonuwu, DHSM, MARS, DG Disease Control and Prevention from MoH, opened the meeting, and he emphasised the need for regular monitoring of implementation of IAR recommendations. Around 100 participants engaged in the IAR monitoring meeting, comprising of MoH, National Disaster Management Authority, Presidential Staff Office, Secretariat Cabinet Office, Ministry of Internal Affairs, Coordinating Ministry of Human Development and Cultural Affairs, COVID-19 Task Force, professional organisations, government partners and stakeholders from multiple sectors. During the meeting, WHO presented an update on the global COVID-19 situation, including measures for enhancing readiness for the Omicron variant. The MoH presented a COVID-19 situation analysis, achievements, and gaps in each response pillar.
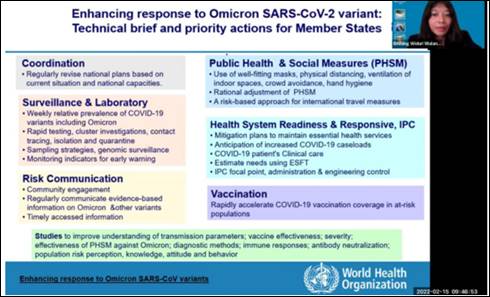
Fig. 2. WHO presented an update on COVID-19 and enhanced readiness for the Omicron variant during the 5th IAR meeting (Credit: Endang Wulandari/WHO)
Achievements highlighted included:
- Updated COVID-19 guidelines, including on the case management pillar.
- Implementation of telemedicine for self-isolation of mild and low-risk COVID-19 cases.
- A network consisting of 15 genomic sequencing laboratories established; the laboratory test capacity reached 2720 samples per month; the laboratory whole genome sequencing strategy has been disseminated. A total of 75 laboratories can conduct S-gene target failure testing to identify probable Omicron COVID-19 cases with a 5256 daily test capacity. 913 out of 977 laboratories have conducted a quality control programme (QC) organised by the national referral laboratory.
- Regular refresher training for COVID-19 surveillance, testing, tracing and monitoring of quarantine with 37 500 tracers and help desk trained. Out of 208 570 people trained for Silacak (contact tracing reporting), 66 776 users are active. 95.3% of districts (490 districts) achieved testing of 1/1000 population per week, while 24 districts have not yet achieved the target.
- Collaboration between MoH and Ministry of Education, Research and Technology, Ministry of Internal Affairs and Ministry of Religious Affairs to develop a policy on implementing COVID-19 protocol in schools and setting up a COVID-19 surveillance system in schools.
- Establishment of adverse event following immunization (AEFI) sentinel surveillance in 14 hospitals in seven provinces.
- Risk communication training, active media engagement, a forum to facilitate multi-sectoral coordination programme for risk communication and counter hoax, deliverable of key public messages for community and operational of COVID-19 hotline.
- Hospital readiness assessment was conducted covering 1111 government, armed force, police and private hospitals. The assessment indicated that infection control implementation has reached 90%.
- Coordination, surveillance, communication, financing, human resources, surge capacity, essential health services, and case management readiness of hospitals capacity were ranging between 83 and 88% while occupational health and psychosocial support readiness stood at 70%.
- A laboratory readiness assessment was conducted covering 373 out of 764 COVID-19 laboratories. The assessment indicated documentation, sample collection and shipment, data and information management, reagent, supply and laboratory equipment management, facility, laboratory testing and biorisk management reached between 91 and 94% capacity. While organisation and management capacity were at 88% human resources and public health laboratory functions between 80 and 84%.
Highlighted recommendations to improve COVID-19:
- Review COVID-19 response plan addressing COVID-19 Omicron variant context including transition and recovery plan at all levels with regular monitoring of response plan indicators, linking to standard minimum service indicators and Ministry of Internal Affairs standard minimum services for disaster response.
- Regular review of logistics needs assessment (e.g., using essential supply forecasting tool), mapping and monitoring the logistic distribution and stockpiling.
- Adaptation of updated WHO guidelines for COVID-19 public health surveillance and contact tracing and quarantine in the context of Omicron SARS-CoV-2 variant.
- Continue strengthening of testing, tracing, and isolation through refresher trainings and mapping of tracers and emergency funding mechanism to support the need for additional tracers.
- Improving data synchronisation and transparency at all levels, improving the completeness and timeliness of reporting and data analysis in collaboration with the epidemiology association.
- Maintaining and improving data quality and sample shipment of influenza-like illness (ILI) and severe acute respiratory infections (SARI) sentinel surveillance and using ILI SARI sentinel surveillance to monitor COVID-19 situation. Conducting WGS from ILI SARI sentinel surveillance as a part of WGS sampling strategy.
- Mapping turn-around time of whole genome sequencing (WGS), monitoring of WGS implementation for timely results and information sharing, including the relative prevalence of COVID-19 variants for comprehensive analysis for risk assessment.
- Sharing weekly cases and mortality data, including age group and cases in healthcare workers and relative prevalence of variants to contribute to national, regional and global risk assessments. Conducting mortality audit for healthcare workers and excess mortality study.
- Implementing solidarity trial plus.
- Develop a hospital readiness plan and monitor of hospital readiness to prepare for a surge of cases.
- Improved systematic cascade trainings using case-based scenario workshops, monitoring and evaluation trainings in infection control and case management, including mapping trainees for deployment roster if needed to respond to increasing cases.
- Monitoring of telemedicine implementation.
- Adoption of Infection Prevention and Control Assessment Framework (IPCAF) for infection prevention control.
- Continue regular surveys on implementing health protocols for COVID-19 in the community to inform the effective risk communication strategy.
- Improving proficiency of lab network quality control, monitoring reagent supply logistics and monitoring implementation of biorisk.
- Monitoring and evaluation implementation of protocols for travel bubbles in International events.
- Continue monitoring public health and social measures using adjusted indicators.
- Development and monitoring of implementation of COVID-19 vaccine deployment plan 2022, improving COVID-19 Vaccine Introduction Readiness Assessment Tool (VIRAT), improving monitoring tracing for vaccine drop out, and revising the risk communication strategy to improve the uptake of vaccination.
The IAR monitoring meetings continuously served as a platform for interactive discussions among stakeholders to discuss lessons learned, identify gaps, and contribute to improving COVID-19 response and building back better health system for public health emergencies in the long term.
***
