Adolescent boys and men
Globally, men accounted for 55% of total new HIV infections among adults in 2023. Outside of sub-Saharan Africa (SSA), men and boys accounted for 70% of HIV infections. In SSA, HIV cascade data shows that men are less likely than women to know their HIV status (85% for men vs 91% for women), initiate treatment (78% for men vs 85% for women), and reach viral suppression (71% for men vs 79% for women).
Global HIV data through 2023 show that progress towards the 95-95-95 targets (95% of people living with HIV know their HIV status, 95% of people who know their status are receiving treatment and 95% of people on HIV treatment have a suppressed viral load) for men lags behind at 83-86-94 compared to 91-94-93 for women. The testing and treatment cascade shows even greater disparity with antiretroviral therapy coverage considerably lower for men than women globally (72% vs 83%).
Across nearly all regions, men living with HIV are less likely to access HIV services, less likely to get tested, less likely to be virally suppressed, more likely to present with advanced disease and consistently fare worse across the HIV testing and treatment continuum.
Gender norms only partly explains why some men delay seeking care, but other factors are also at play. In many resource-limited settings, health systems are largely designed to address critical maternal and child health needs. Similar entry points for men are not commonplace.
It is important that we recognize and reach men in all their diversities including key populations such as people who inject drugs, people in prison and men who have sex with men who face numerous social and structural barriers to care, and those who have been previously excluded from health services.
Voluntary medical male circumcision (VMMC) is an important entry point for providing men and boys with broader, more appropriate health packages. Since VMMC was recommended by WHO and UNAIDS in 2007 as key to HIV prevention in high-prevalence settings, about 37.5 million men have accessed services across 15 priority countries in sub-Saharan Africa. This has contributed to averting new infections and related healthcare costs.
We need to shift away from blaming men for poor health-seeking behaviour. Men need, are willing and deserve to have access to services. Focused efforts are needed to reach and engage men to stay free from HIV, get tested regularly and start and stay on treatment. This will both improve male health outcomes and contribute to declines in new HIV infections also among women and girls.
News
Publications


/global-hiv-hepatitis-and-stis-programmes-(hhs)/alarming-decline-in-adolescent-condom-use-20183615.jpg?sfvrsn=aa46600c_4)


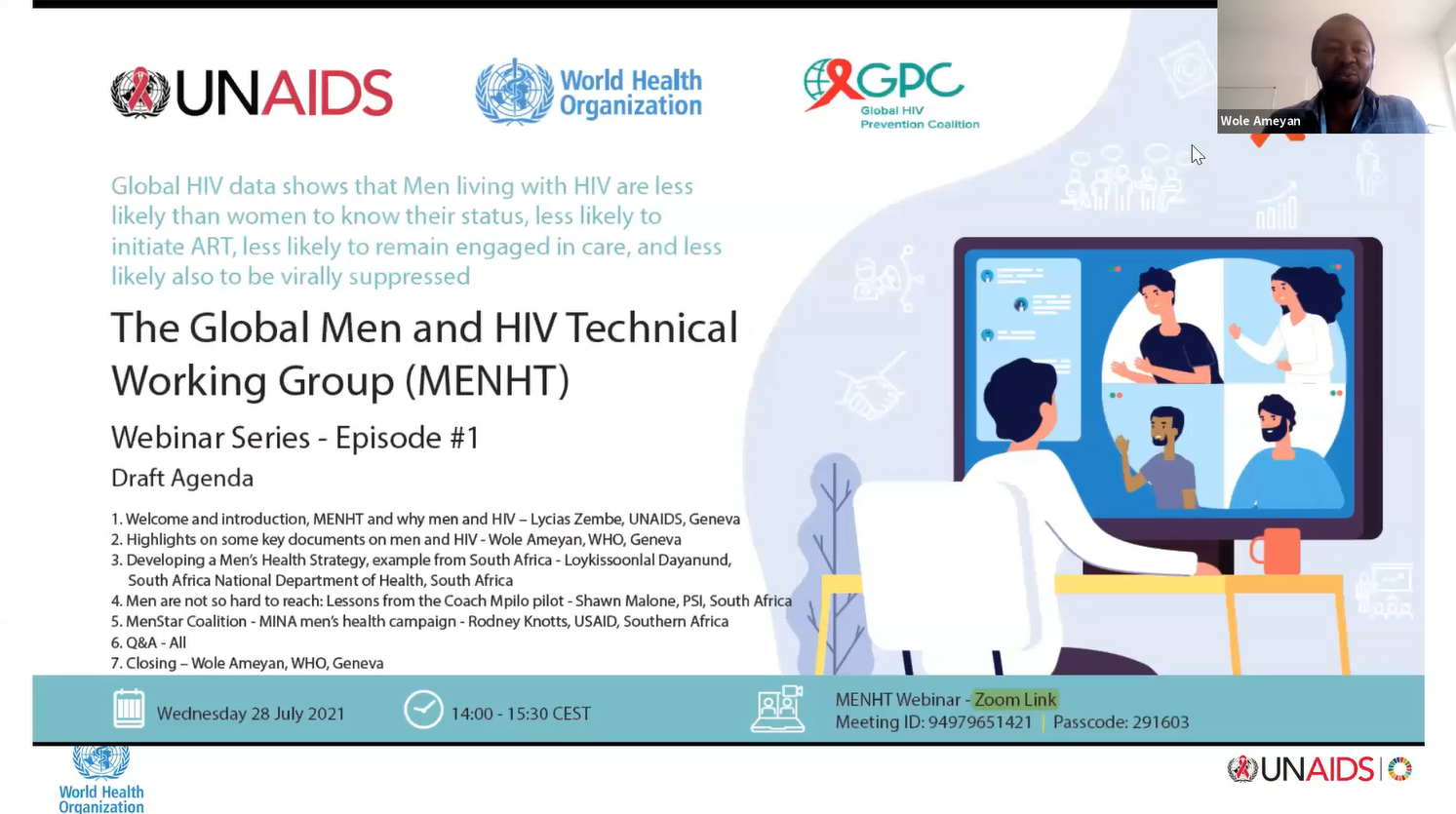 Episode 1 - 28 July 2021
Episode 1 - 28 July 2021